You are currently browsing the category archive for the ‘Wellbeing’ category.
Following last week’s post about how my ADATS’ talk was received, several things happened. Firstly, I was contacted by a heap of people wanting to chat about the reaction. Secondly, I was sent several designs of logos and t-shirts with ‘deliberately non-compliant’ splashed across the front, which obviously I will now need to order and wear any time I do a talk (or am sitting opposite a diabetes healthcare professional). And thirdly, discussions started about how we manage our diabetes ‘off label’.
While off label generally refers to how drugs are used in ways other than as prescribed, it has also come to mean the way we tweak any aspect of treatment to try to find ways to make diabetes less tiresome, less burdensome, less annoying.
When it comes to making diabetes manageable and working out how to fit it into my life as easily and unobtrusively as possible, I am all about off label. And I learnt that very early on.
‘Change your pen tip after every use.’ I was told the day after I was diagnosed, meeting with a diabetes educator the first time. ‘Of course,’ I said earnestly, staring intently at the photos of magnified needles showing how blunt the needles become after repeated use. ‘Lancets are single use too.’ I nodded, promising to discard my lancets after each glucose check. ‘You must inject into your stomach, directly into the skin – never through clothes, and rotate injection sites every single time.’ I committed to memory the part of my stomach to use and visualised a circular chart to help remind me to move where I stabbed.
Fast forward about a week into diagnosis. Needle changed once a day (which then, in following weeks, became once every second day, every third day, once a week… or when ‘ouch – I really felt that’); I forgot that lancets could be changed; speared (reused) needles directly through jeans or tights into my thighs, having no idea which leg I’d used last time.
And then there were insulin doses. ‘You must take XX units of insulin with breakfast, XX with lunch and XX with dinner. That means you need XX grams of carbs with breakfast, XX with lunch and XX with dinner. These amounts are set and cannot be altered. You must eat snacks.’ I took notes and planned the weekly menu according to required carb contents. Within a week, I’d worked out that if I couldn’t eat the prescribed huge quantities of carbs, I could take less insulin and that all seemed to work out okay. And I worked out how I didn’t need to have the same doses each and every day. It was liberating!
I switched to an insulin pump and the instructions came again: ‘You must change your site every three days without fail.’ I promised to set alarms to remind me and write notes to myself. ‘Cartridges are single use,’ I was told and vowed to throw them away as soon as they were empty. Today, sometimes pump lines get changed every three days, sometimes three and a half, sometimes four and sometimes even five. Cartridges are reused at times…
I was also told to never change any of the settings in my pump unless I spoke with my HCP. But part of getting the most from a pump (and all diabetes technology) is about constantly reviewing, revising and making changes. I taught myself how to check and change basal rates – slowly and carefully but always with positive results. (For the record, my endo these days would not tell me to never change my pump settings.)
CGM came into my life with similar rules, and as I became familiar with the technology and how I interacted with it, I adapted the way I used it. Despite warnings of never, ever, ever bolusing from a CGM reading, I did. Of course I did. I restarted sensors, getting every last reading from them to save my bank balance. I sited sensors on my arms, despite warnings that the stomach was the only area approved for use. I started using the US Dex 5 App (after setting up a US iTunes account and downloading from the US App Store) because we still didn’t have it here in Australia, and I wanted to use my phone as a receiver, and seriously #WeAreNotWaiting.
And today…today I am Looping, which is possibly the extreme of using devices off label. But the reason for doing it is still the same: Trying to find the best ‘diabetes me’ for the least effort!
The push back to curating our diabetes treatment to fit in with our lives is often frowned upon by HCPs and I wonder why. Is it all about safety? Possibly, but I know that for me, I was able to always measure the risk of what I was doing off label and balance it with the benefit to and for me. I believe I have always remained as safe as possible while managing to make my diabetes a little more… well, manageable.
It can be viewed as rule breaking or ‘hacking’. It can be thought of as dangerous and something to be feared. But I think the concerns from HCPs go beyond that.
As is often the case, it comes down to control – not in the A1c sense of the word, but in the ‘who owns my diabetes’ way.
When we learn how things work, make changes and adapt our treatment to suit ourselves, we often find what works best is not the same as what we are told to do. And I think that some HCPs think that as we take that control – make our own decisions and changes to our treatment – we are making them redundant. But that’s not the case at all.
We need our HCPs because we need to be shown the rules in the first place. We have to know what the evidence shows, and we need to know how to do things the way the regulators want us to do them. We need to understand the basics, the guidelines, the fundamentals to what we are doing.
Because then we can experiment. Then we can push boundaries and see what is still safe. We can take risks within a framework that absolutely improves our care, but we still understand how to be safe. I understand the risks reusing lancets, or stretching out set changes by a day or two. Of course I do. I know them because I’ve had great HCPs who have explained it to me.
Going off label has only ever served to make me manage my diabetes better. It has made me less frustrated by the burden, less exasperated by the mundanity of it all.
And the thing that has made me feel better – physically and emotionally – about diabetes more than anything else is using Loop. So, use it I will!

It seems silly to have to say this, but I will anyway. Don’t take anything I write (today or ever) as advice. I’m not recommending that anyone do what I do and I never have.
Helen Edwards from Diabetes Can’t Stop Me has written a thoughtful piece today on her blog about why she has ‘broken up with CGM’.
I truly love this post, because it once again reinforces the ‘one size fits no one’ approach that I have always advocated when it comes to diabetes.
As I read Helen’s story, I realised I could have written this post. I was reminded of the long and very winding road that it took for me to get to a point where I could live comfortably with all the tech. Learning to love it took even longer. It certainly was not love at first sensor! For a long time, I felt overwhelmed by all the data, the alarms drove me to distraction and I struggled at times to live with an invisible condition when all my robot bits are on show.
I showed the below photo during my talk at ADATS last week. It’s from a few years ago (and accompanied this post) when I was really struggling to live alongside CGM. I had to work up to convince myself to put on a sensor and made all sorts of deals to try to limit the stress I was feeling. I turned off all the alarms except for the low alarm. I promised myself that I would rip the sensor out if I was starting to be paralysed with all the information being constantly thrown at me. And I reminded myself that the data was just numbers trying to retrain my brain to not feel judged by the electronic device.

This wasn’t the first time I made such a deal with myself. And it took this and many other attempts of starting to wear CGM before everything feel into place. There were times where I pulled sensors out after two days because I just couldn’t cope with it.
Learning to live alongside diabetes technology is not an easy decision. There is bargaining, sacrificing and trade-offs. The tech is brilliant, but it rarely, if ever, works as simply as the shiny brochures promise. It’s not perfect and the limitations of the technology should never be blamed on the person wearing it.
Also, it’s no good speaking to people like me, because I’m all evangelical about it and spend all my time telling people how much I love it – while conveniently forgetting how long it took to find that place.
The tech is not for everyone and no one should be made to feel bad if they choose a more analogue approach to diabetes management. This is another slide I showed at last week’s ADATS meeting (from this post):

Right device; right time; right person. The right device might actually be no device at all. And that is absolutely fine!
Are you an adult (aged 18 – 75 years) with type 1 or type 2 diabetes living in Australia or the UK?
No? Avert your eyes and go back to looking at pictures of of cats on the internet.
Yes? Stop right there…. You can go back to looking at pictures of cats later, ‘cause right now, you have better things to do.
Like THIS:
YourSay (Self-management And You): Quality of Life Study needs people just like you to have your say about the impact of living with, and managing diabetes on your quality of life.
You only have until the end of the month to participate, so now is definitely the time to do it.
And to say thank you, I baked these and am virtually sending you a couple:

You’re welcome!
At #DX2Melbourne last week, we had a live webcast in an attempt to include people not invited to be part of the event to hear from some of the bloggers and contribute to the discussion. The hour-long webcast was about diabetes and mental health.
With delusions of Jenny Brockie and Tony Jones, I facilitated the discussion – which was actually quite difficult as there were thirteen of us sitting in a row meaning we couldn’t all see anyone other than who was sitting directly next to us without leaning dangerously forward. Also, I kept nearly falling off my stool, which suggests that I am the most ungraceful creature to have ever been positioned in front of a camera.

I’d put together some questions and discussion points to guide the discussion, but was very open to any tangent the group wanted to take to really navigate and explore the topic of diabetes and emotional wellbeing.
As the discussion flowed, I couldn’t help but feel a sense of déjà vu. Another talk about how diabetes affects us emotionally; another talk about not getting the support from psychologists and counsellors that we need; another talk about how usually it’s not even recommended that we may need to speak with someone about the mental health aspect of living with a chronic health condition; another talk from well-connected diabetes advocates saying that there is more to diabetes than simply being told our A1c, or any other number for that matter.
Amongst all the chatter, I asked myself how many times I’d participated in talks, how many talks I’d given, how many tweet chats I’d tweeted in, how many blog posts I’d written that were about the emotional side of diabetes. And then today, on my TimeHop app came this tweet, from an OzDOC tweet chat about mental health, held exactly 12 months ago today:

I’m not saying this because I think we’ve ‘done’ this topic and should leave it alone now. Not at all. I’m just suggesting that we’ve been having the same discussions about this really important topic for a long time, and yet diabetes care still seems to have this imaginary, yet somehow real, line down the middle, with the physical aspects of diabetes to one side, and the emotional aspects on the other as if the two are not fundamentally connected.
I knew that there would be some people listening in who would be hearing all of this for the first time. It would be the first time that although they had probably worked out that there was something missing from their diabetes care, they weren’t sure what it was. Or, they may have known they needed to speak to a psychologist or a counsellor, but didn’t know who to ask about it…and anyway, they may have thought, surely if this was something that lots of people with diabetes feel, someone would have mentioned it by now, right? Right???
Nineteen years I’ve had diabetes. And for at least seventeen of them, I’ve understood and known the importance of checking in on how the emotional impact of diabetes is contributing to how I am managing my diabetes. Or how I am not managing my diabetes (see above tweet….).
The idea that we can separate our mental health and emotional wellbeing from our diabetes is ridiculous. A condition that permeates every aspect of our life, moves in, makes itself a home and lords over us with terrifying threats of what lies ahead, impacts on our abilities to manage the day-to-day physical things we need to do.
Those watching the webcast at home could submit questions for the panel. A couple of diabetes healthcare professionals were watching and one asked a question that, as I read it, made my heart sink. He said that he sees people with diabetes who he believes would benefit from seeing a psychologist, but he is concerned that they will be offended if he suggests it. He asked the panel for ideas on how to broach the subject without causing offense.
Why did my heart sink? Because the question showed that there is still so much stigma associated with seeing a mental health professional, that other HCPs – on the ball, sensitive ones who know and understand the intersection between diabetes and mental health – feel worried that they might upset someone with diabetes if they suggest referring to a psychologist.
Until we normalise psychological support – until at diagnosis when we’re introduced to our new diabetes HCP best friends and psych support is part of that team – the stigma will continue. I’m not suggesting that everyone will need or want to see a psychologist. But putting it on the list, alongside a dietitian and a diabetes educator and an eye specialist will at least people understand that, if needed, there will be someone there to help with that particular piece of diabetes. (And to be perfectly honest, I really do wish I’d seen a psychologist at diagnosis rather than the dietitian who has scarred me for life with her ridiculously large rubber-mould portions of carbohydrate she insisted I eat at every meal!)
I don’t feel as though I am a failure because I have needed to consult a mental health professional in the past. I don’t think that it suggests that I can’t cope or that I can’t manage diabetes. I see it as important a part of my diabetes management as anything (and anyone) else. A lot of the time, I don’t feel as though I need to see someone. But other times, I do. And that is fine.
DISCLOSURES
Abbott Diabetes Care covered all my costs to attend #Dx2Melbourne, and provided all attendees with two FreeStyle Libre sensors and, if requested, a scanner. There was no expectation from Abbott that I would write about the event or any of their products, and everything I do write about it is my opinion, in my own words, and in no way reflects those of Abbott – or anyone else, for that matter.
You know that old word play about why we should not assume anything? Because ‘assume’ makes an ‘ass’ out of ‘u’ and ‘me’. Yes, it’s lame and I don’t like using ‘u’ for ‘you’ (because I’m a word nerd and don’t do ‘text speak’), but the sentiment is good.
There are so many assumptions that come with diabetes. And almost all of them are destructive.
‘People with diabetes must have eaten too much <insert food/drink type> as a kid.’
‘People get diabetes because they’re fat.’
‘People get diabetes because they don’t exercise.’
‘Diabetes means you are sick.’
‘People with diabetes could be managing better if they just tried.’
Many of us will have had these sorts of comments made directly at us. Some of us will have heard people say these things. Most of us will have seen these sorts of comment perpetuated in the media and in popular culture anytime diabetes gets a mention.
And they are all wrong.
It’s time that we removed all negative assumptions and replaced it with just this:

Imagine how different things would be if that was the starting point of diabetes discussions. Instead of the judgement and finger pointing that often is associated with a diabetes diagnosis, the first thing that everyone said was ‘And now let’s talk about living well with it.’ Instead of the threats, the attitude was ‘You can thrive with the right treatment’.
Finding out someone has diabetes does not in any way give you a window into their life or an indication into their behaviour. But it does tell you that they have a health condition that requires regular management and the best possible treatment.
Imagine how much easier life with diabetes would be – and how much kinder the conversation would sound – if the next time we told someone we have diabetes, the only thing we heard was ‘Are you getting the healthcare and treatment you need?’
Wouldn’t that be a great place to start the conversation?
If you can, think back to when you were diagnosed with diabetes. Can you remember much of it?
I can. I can remember almost every word that the endo, diabetes educator and dietitian said to me. I can remember that, in amongst the explanations of what diabetes was all about and how it would impact on my life, there were thinly-veiled threats about what would happen if I strayed from the plan I was being given with the expectation that I would follow it. I remember the rigid ‘my-way-or-the-highway’ instructions about how life with diabetes would be.
But mostly, I remember what was missing. There was no mention about the impact of diabetes on my emotional wellbeing. No one suggested that speaking with peers – others living with diabetes – might provide me with some much need comfort or camaraderie. No one hinted that I might like to do some of my own reading and investigating to come up with my own ideas of how to best manage this chronic condition that had moved into my body, my mind, my life.
No one told me there were options or suggested that I needed to carve out my own path and then work out to navigate it best.
If only I’d had a guide to help me do that – something to give me some ideas that felt more in line with how I lived before diabetes. I wanted something that shared real-life experience about how to make diabetes fit into an already really busy life, and help me be conscious of making healthier choices, but choices that didn’t feel as though they were suffocating me.
Now I have it – albeit 19 years too late!
Adam Brown from diaTribe has written Bright Spot and Landmines which he has sub-headed ‘The Diabetes Guide I Wish Someone Had Handed Me’.
As I read this book, I started to think about how different those early diabetes years would have been for me – the years before I found my voice, my people and an ability to work out my own way with diabetes.
I could use words such as ‘sensible’ and ‘practical’ and ‘level-headed’ to describe the advice gently doled out in Adam’s book, and they would all be accurate.
But they would be underselling the value of the book.
Adam highlights the landmines – the things we all do to take short cuts – that inevitably negatively affect our diabetes. Often we think these short cuts save us time or ‘fix’ a diabetes problem quickly, only to find that they often turn out to be time consuming and actually end up causing more problems than the original one we were trying to address.
The bright spots are suggestions on how to positively and sustainably live with diabetes. They are easy to manage, and don’t ask for a significant shift in thinking, or large financial or even time investment to make the changes.
The book is segmented into four sections: Food, Exercise, Mindset and Sleep. This makes it super easy to use as a reference book and dive into it to help target specific areas that you want to think about. I’ve read the whole book through twice now, but keep going back to the sleep section, because I realised that it is an area of my life that I really need to address now.
I honestly wish that the day I’d been diagnosed with diabetes I’d been handed this book. I wish I’d had it on my shelf all those years as a resource to refer back to in moments of burnout or no motivation, or when I needed a little push to encourage me. I wish I’d been able to tap into Adam’s wisdom on specific issues when I was struggling with being in a food rut that was affecting my glucose levels, or in a funk because my mind was not clear or focused.
I’m so glad to have it now and have already made some changes which have been very positive. It might be 19 years late to the party, but this book will be on my shelf to be pulled down very, very often.
It doesn’t matter how long you’ve had diabetes; you WILL get something out of Adam’s book. But if you or a loved one is newly diagnosed, I would recommend you stopping whatever you are doing RIGHT NOW and getting a copy. You can buy a paperback copy here, or download the PDF here, naming your own price.
If you would like to win a copy of Bright Spots and Landmines, I can hook you up! Adam generously provided me with some copies when I caught up with him recently at ADA. Just click here and tell me in 25 words or fewer why you would like to win a copy of Bright Spots and Landmines. But chop chop! You’ve only got until the end of the weekend to enter.
In my endo appointment the other day, after we’d finishing working through my pathology results, I wanted to speak about the mythical pre-bolus.
I say mythical because, seriously, the day I work out how to get the whole pre-bolus thing right is the day I see a unicorn walking up a rainbow while talking to a phoenix. I have hope this will happen one day.
My endo is one of those rare beings who understands the absolute intricacies of pumps. She knows a lot – from simple button pushing to complex things that make my brain hurt. When I started talking pre-bolusing, she brought out graphs and charts to help us work through my questions.
I mentioned that eating lower carb certainly helps avoiding post-meal spikes, but I was having trouble getting my morning coffee dose right. I know exactly the number of carbs in the milky-latte-with-one I order, but the timing of the bolus is critical to avoid a post-caffeine spike and ensuing plunge.
‘Plus,’ I added. ‘It depends what is going on with my glucose level as I start to drink. If I’m already dropping, which may be happening at that time of morning, and I bolus too early, I’ll end up hypoing, so I usually wait until about five minutes before I order my coffee. But if I’m above target, I need to bolus at least 15, but more like 20 minutes before ordering. If I’m steady and in range, somewhere closer to 10 is more like it. Maybe 12…’

Just drink the damn coffee!
I heard myself going into such detail and suddenly, I realised how bloody boring I sounded. My poor endo had just endured a 10-minute monologue from me on bolus dose timing to cope with my over-priced morning coffee from the hipster coffee shop next to work. I couldn’t help wondering if this really is the best use of the time and expertise of a most excellent endocrinologist? Also, I was embarrassed at presenting this first world problem as such a pressing issue.
She showed me some graphs, and drew a few others for me to think about. We spoke about timing and strategies and things to consider before pressing the bolus button.
But then she stopped and said, ‘You know, you can think about all these things, but you can also not worry too much. Obviously it’s up to what you want to do here, but thinking about things in ‘minutes’ before your dose…you need to decide if that really necessary.’
And then it hit me. The over-analysing and over-stressing and excessive scrutiny. What for? I’d just seen an in-range A1c that suggested I’m managing just fine with what I’m doing. Was the angst of blousing twelve minutes versus 16 minutes prior to my morning caffeine jolt really worth the calculations and the strain?
We are often critical that our HCPs put unreasonable expectations on us with what they demand we do to manage our diabetes. How refreshing to have a diabetes HCP who actually suggests that we breathe and take a step back for a moment to decide if a particular undertaking is absolutely necessary, or if it is just adding unnecessary pressure to our already highly-pressured diabetes selves.
It’s day four of the eighth annual #DBlogWeek, created by Karen from Bittersweet Diabetes. This is the sixth year I’ve taken part and it’s a great opportunity to not only write about some truly interesting topics, but also a chance to read some blogs you may not otherwise. Here are the links to today’s posts.

Today’s prompt: May is Mental Health Month (in the US) so now seems like a great time to explore the emotional side of living with, or caring for someone with, diabetes. What things can make dealing with diabetes an emotional issue for you and / or your loved one, and how do you cope?
One of the things I’ve found about living with diabetes is that the way I respond to certain situations is inconsistent. Some days, I’ll look at a rollercoaster CGM trace, shrug my shoulders and think ‘That’s diabetes!’ and move on. Other times, I’ll look at a similar rollercoaster CGM trace and burst into tears, wanting to curl up in the corner under a quilt, asking ‘Why? Why? WHY?’ while someone brings me a cup of tea and Lindt orange chocolate.
There are periods when my resilience stores are high and I can manage anything thrown at me, and other days where the smallest diabetes issue sends me into a spiral of despair. The unpredictability of diabetes is matched only by my own haphazard responses.
There do seem to be some things that do get me down pretty much any time they happen. When diabetes starts to affect my family, making my health issue theirs, I get very emotional and upset. I think it is probably a combination of sadness, guilt, anger and frustration that guarantees an emotional response.
The unknown of diabetes worries and scares me. I don’t think about it most of the time – I guess that is how I cope. The fears and anxiety are neatly packaged up and hidden away, brought out only in moments of weakness – or perhaps when my resilience is low.
Earlier this month, when I was an invited speaker at the Primary Care Diabetes Society of Australia (#PCDSAus) conference, and in the same session as me was Dr Christel Hendrieckx from the Australian Centre for Behavioural Research in Diabetes. Christel was very clear that clinicians need to consider diabetes and emotional health side by side as the two are undeniably connected.

I truly think that when we break it down, we can’t separate the two. When we live with a condition that is so ever-present; that we invest so much of our time and energy into managing; that we can’t put in a box when we are feeling over it and come back to it when we feel more equipped, it’s impossible for it to not impact emotionally.
We, all too often, draw a line with the physical on one side and the emotional on the other side. That line is terribly blurred – if it’s even there at all – when it comes to diabetes.
Brutal. That’s the way I’ve been describing my week. It’s been super busy and there is no hint that will change any time soon.
But there is so much stuff out there to read. Here’s just some of it…
CGM
Oh, did you hear? CGM is now funded for children and young people under the age of 21 who meet eligibility criteria. It’s been ALL OVER the interwebs, but for the most up-to-date info, go here!
(And yes, I know, people 21 and over need CGM and need support. This isn’t over yet…!)
A psychologist who knows diabetes? Yep!
A good psychologist is worth their weight in gold. A good psychologist who understands the impact of living with diabetes on our overall wellbeing is like a unicorn – rare and magical.
So, I was delighted when someone from my office who has been a Research Fellow with the ACBRD for a number of years came to tell me that she is starting a private psychology practice. Dr Adriana Ventura’s research has focused on the psychological, social and behavioural aspects of living with type 1 and type 2 diabetes.
Adriana understands that living with diabetes (and other chronic health conditions) can be challenging. And she understands that these challenges can make it tough to take care of our health the way we would like.
Details about Adriana’s practice can be found here. (Adriana works with adults and older adolescents – 16 years and over)
Really? REALLY?
Seems that we’ve all been doing diabetes wrong. That lancet thing that we joke about never changing? This is how you use it according to the pic accompanying a BBC Radio 2 tweet.

Apparently it is really hard to do some decent research. (And if the image wasn’t enough of a deterrent, the article looks shit too, so didn’t bother reading it.)
My maths teacher was right
So, as it turns out, I do use maths every single day. Diabetes has certainly put my algebra skills to good use!
This article from The Conversation is all about how an applied mathematician developed an algortithm to help treat diabetes. As you do.
Words that over-promise
I can’t remember the number of times I’ve heard that a diabetes cure is ‘just around the corner’ or any other version of ‘five years away’.
But how do these promises affect people living with health confitions? This article from Medivisor asks just that.
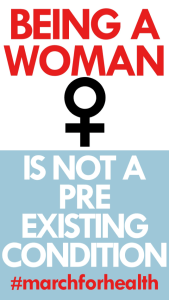
March for Health
While we were celebrating the CGM announcement on Saturday, I was very mindful that my US friends were getting ready to continue their battle for fair healthcare. March for Health was held across the US on 1 April calling for affordable access to quality health care for all people. I don’t know about you, but that doesn’t sound unreasonable to me.
Check out more at the website here.
And this, by the way, is possibly one of my favourite promotional posters from the March.
Women’s Health Survey … Quick!!!
And while we’re talking women’s health…There are still a few days left to do the annual Jean Hailes Women’s Health Survey, which identifies gaps in current knowledge when it comes to women’s health.
College Diabetes Network
There are some really wonderful groups out there supporting people with diabetes, and my friend from the US, Mindy Bartleson emailed me with some really useful information about the College Diabetes Network (CDN). The Network empowers and connects young people with diabetes and their are CDN Chapters on college campuses across the US.
The Network is certainly US based, but some of the information will be relevant to those in Australia (and elsewhere). Their resources provide information about how to prepare for the transition from high school to college or university. Do have a look!
Information for students can be found here. And information for parents can be found here.
I made these cookies and jeez were they delicious!

They are gluten free, which I know is important for many people. For me, I need cookies that take no more than 10 mins to mix together and then taste perfect. Honestly, they are possibly the best tasting biscuit/cookie I have ever made… and I bake a lot.
The recipe can be found here. (I used smooth peanut butter as the recipe suggests, but I reckon they would taste awesome with crunchy. Also, do pop the mixture in the freezer before trying to shape the cookies. The dough is mighty-soft and sticky, and this step helps to get the dough from the bowl onto your cookie tray. AND DON’T SKIP THE SALT ON TOP!! This is what ties it all together and makes the magic happen!)
And finally……
… a little New Yorker Cartoons funny, which may not be directed at diabetes, but boy it certainly shows how I feel most days living as a diabetes tech cyborg!

I’m still getting my head around the #HealtheVoicesAU conference – there was so much that happened over the event that it’s taking time to write about it all and really nut out what I took away from each session. (Previous posts here and here.)
When I looked at the program, I was probably most excited to hear from Nick Bowditch. I knew nothing about Nick other than what the program told us: He is the only person in Asia Pacific to have worked at Facebook and Twitter; he’s an entrepreneur who helps small businesses here and across the globe shape their online presence. And his personal health story is that Nick is a mental health advocate as someone who has lived with depression for many years.
I knew Nick’s talk would have lots to offer, and title of his talk that had me excited: ‘The Art of Storytelling’.
I’ve written before about why I love story tellers and story-telling. And telling my own story. It’s reading and hearing the stories of others with diabetes that helps put in context my own experiences. Others’ perspectives shape my own and I learn so much from how others deal with the clusterfuck that diabetes can be.
The first slide Nick showed us was of the wonderful Jamaa el-Fna in Marrakech. He told us how he spent an evening captivated in the square. There amongst the snake charmers and the men walking around with monkeys on leads and the little girls selling tissues and the vendors hawking fresh orange juice, were story tellers. And although he couldn’t understand a word they were saying, he was enthralled as they animatedly told their stories.
That’s the beauty and magic of a good story teller – you don’t necessarily need to understand the detail; just getting the gist of the tale is enough.
And then, Nick gave us the snapshot of his story. In a nutshell, he told us this:

Slide from @NickBowditch
It’s easy to make assumptions and think that you know what Nick might be living with if you see that list. But you’d probably be wrong. I know I certainly was. My initial ideas of what life must be like for Nick were turned on their heads as he put into context what each of the above aspects of his life actually means to him:

Slide from @NickBowditch
By turning our assumptions on their head and reframing how he lives with mental health conditions shows us that Nick is not ‘just coping’, he’s living. His words were: ‘These are not my defects. These are my superpowers.’ And it challenges us to reconsider our preconceived ideas. I know that those of us who speak about diabetes often challenge what others think.
The image of T1D being all about kids and needles and blood is not really what it’s about for me. And the far-too-easy idea that T2D is all about older, overweight, inactive people is wrong too.
When we tell our stories – and reframe the narrative – the truth comes out.
Possibly the most powerful thing Nick said was this: ‘Telling the truth is not brave. It’s easy. The hard thing is not being authentic.’ We’d come full circle back to the first speaker of the day who implored us to find authenticity in what we were saying. And it reminded me of why I have always been an advocate of having people with diabetes sharing their stories in any forum where people are talking diabetes: the legitimacy of lived experience cannot be found in any other way than actually having someone tell their story.
I see first-hand the power that having a person with a health condition stand alongside a healthcare professional and put into context the theory and research that they have just presented.
There is an art to storytelling. We do it every day that we tell our story. We do it every time we put words on a page for a blog post, or in a diary or in a letter, ot when we stand up and tell it like it is. Some do it far more elegantly and eloquently, but the things is; it doesn’t matter. As long as we’re authentic.

DISCLOSURE
Thanks to Janssen (the pharma arm of Johnson and Johnson) for covering my travel and accommodation costs to attend the #HealtheVoicesAU conference. There was no expectation by Janssen that I would write about the event and everything expressed here (and on Twitter Facebook and other social feeds) is mine and mine-alone! To read more, check out the conference hashtag, #HealtheVoicesAU, on the socials.








