You are currently browsing the category archive for the ‘DOC’ category.
For more information (all Australian sites):
Diabetes conferences and scientific meetings in 2020 have looked very different than in previous years. It looked as though we were off to a flying start with a successful ATTD in Spain back in February. But not long after all the attendees returned to their corners of the globe, the world turned upside down and decided that, along with everything else, in-person meetings were done.
Major professional conferences such as those run by ADA, DUK, EASD, ISPAD, ADS & ADEA and IDF have all either happened, or will be happening, virtually, with a Zoom (or other) platform being where we meet, rather than a massive conference centre in a major city.
As ever, I search for a silver lining and if there is one it is this: the pivot to virtual conferences means that some of the main barriers in the way preventing PWD attending diabetes conferences are somewhat reduced. With travel, accommodation and a lot of the other expenses out of the way, it may be easier for advocates who would like to attend to find their way in. Let’s look at that as the disruption we needed to have to get PWD flocking to meetings in droves.
There is still the matter of registration passes, and we know that is not always the easiest thing to overcome. The registration fee is significant, and some conferences only allow HCPs and researchers in. Usually, press passes provide a way to get passed security, but they require letters of assignment (sometimes from diabetes organisations who ask PWD to act as ‘on the ground’ reporters), or other criteria be met. And, of course, there are invitations to attend satellite events extended from device and drug companies to some advocates. While there is often criticism at these methods, they have meant that there are PWD at conferences, many of whom provide information back to the community.
At ATTD, there was a new way in. Advocacy group #dedoc° launched a new program, #dedoc° voices, which you can read all about here. For the pilot of the program in Madrid, the diabetes advocates whose applications were successful had access to all parts of the meeting.
#dedoc° voices is happening again for EASD (coming up next month), and it’s not too late to apply. And as an added bonus, successful applicants will also receive registration to the ISPAD conference in October. ISPAD is the International Society for Pediatric and Adolescent Diabetes, so if you are a parent of a kid with diabetes involved in advocacy and peer support, you may be super keen to attend this one.
To apply, go here. #dedoc° voices is open to PWD now, so if you have always wanted to attend a major diabetes conference, there is nothing stopping you from applying, right now. Any one from anywhere around the world can apply – the only consideration is how you’ll manage time zone horrors if you don’t live in the same zone as the conference. (But please don’t come crying to me about that – I’ve spent the last six months settling in for hour long meetings hosted out of Europe of the US which begin long after sunset and involve perky people just waking up while I yawn and struggle not to fall asleep in my Zoom square!)
What are you waiting for? Apply now and come be a part of one of the biggest diabetes meetings in the world. I promise there will be lots of other PWD there for you to (virtually) meet up, and share ideas with. Come say hi!
Disclosure
I am an advisor to the #dedoc° voices program. I do not receive any payment for this role. 
Spend enough time trawling through social media posts with a #DOC somewhere in the hashtag, and it is inevitable that you will see photos of people’s CGM graphs. Often, it’s PWD getting excited at their flat line graphs because they have managed to stay within range for a certain period of time. Or perhaps it’s to show shock and utter disbelief at loop systems doing all the work. It can be because we won’t to show how we have managed to nail the timing and amount of a bolus, and that usually-difficult to manage food nemesis (hello, rice!), completely avoiding a spike. Or, it could be just because we feel like sharing.
I don’t share my graphs a heap these days, but have in the past. It’s a personal decision as to whether we want to share their data online, and if you do, knock yourself out. Your data, your rules! I understand why some feel that it can be considered not especially helpful for others, setting us up to feel we are failing if we compare. But the conversation sharing can generate is really useful for a lot of people.
Every now and then, a non-PWD will share their libre or CGM trace to show that even those with a perfectly working pancreases are subject to glucose fluctuations. This is done with the intention of support and encouragement and to show that flat lines really are unrealistic. While I’m sure that those sharing glucose graphs of people without diabetes is never done with any malice – in fact, completely the opposite – I believe it is nonetheless problematic, and misses the point.
I get it. It’s a noble goal to try to make PWD feel less negative when we are unable to manage a perfectly flat line at 4.0mmol/l for hours on end. And to also understand that’s not how the body actually works, even when everything is doing what it should be doing.
But it is totally redundant. And downright annoying. And also, completely inconsiderate.
I live with diabetes and am fixated on trying to limit the variation of my glucose levels because I have to. PWD are told that keeping those numbers between 4mmol/l and 8 mmol/l is the goal. And we’re told that when we go outside of those numbers – especially when we go beyond the upper limit, all manner of nasty things will happen to us. That’s what was told to me the day I was diagnosed with diabetes, and repeatedly what I have seen since.
Showing me your graph that just happens without any effort on your part is not reassuring. It’s pointless. And somewhat heartless. When your level goes up to 12 because you ate a family block of chocolate, it comes back in-range fairly quickly. And not because you had to do any fancy-pants calculations, or micro (or rage) boluses.
When I eat a block of chocolate, whatever happens next is pretty much 100% due to my efforts. I have done some fancy pants calculations. I have had to bolus – maybe once, most likely a number of times – to get my glucose level back in range. And then I sit there and hope that I haven’t over bolused…
Oh – and when you show me that your glucose levels dipped into the low range or sat there for a while, it doesn’t reassure me or make me feel ‘normal’. Because the difference is that when that happens to me, I am doing all I can to make sure that I am okay, that I don’t pass out, that I don’t overtreat (again!), and that I am safe. And then I get to recover from a hypo hangover – something you are fortunate to never experience.
To be honest, I actually find it completely ironic when it is HCPs sharing their data to make me feel better, and a little thoughtless because the reason that I am in constant pursuit of these straight, tightly-in range lines is because it is HCPs that told me in the first place that is where I must stay to ‘prevent’ all.the.nasty.things.
And finally, when this happens, it centres people without diabetes in a conversation that should very much have the spotlight firmly shone on us. Your glucose level data, and the patterns they make are not like ours. They do not represent the blood, sweat and tears, the emotional turmoil, the frustration, the fear that that is somehow reflected in our data.
Perhaps rather than sharing non-PWD data, instead acknowledge just how difficult it is to do diabetes, and commend people with diabetes for showing up, day after day, to do the best we can – regardless the shape of our CGM graph.
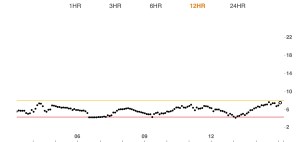
A real-life PWD CGM graph. Mine, from about 10 minutes ago.
One of the things the diabetes community does best is come together in tough times, and this new initiative from JDRF and Beyond Type 1 is a stellar example of how it can be done. JDRF and Beyond Type 1 formed an alliance last year, and have put together a terrific site providing important, up-to-date information and advise about coronavirus and diabetes.
But this is initiative goes way beyond just two diabetes organisations. In fact, over one hundred diabetes organisations, charities, and companies are helping to spread the word and share the information via their networks
Charities and diabetes organisations from Australia, USA, Canada, Italy, Chile, Portugal, Mexico, Bulgaria, Germany, India, Cyprus, New Zealand, Spain and other countries too are represented. I’m thrilled that Diabetes Australia is one of the community partners on the ever-growing list!
International organisations such as Life for a Child, ISPAD, IDF, NCD Alliance as well as industry partners have also rallied together, joining the other groups. This is big. Big! Huge!
The information on this new site is simple and clear. And it’s available in English, Spanish and Portuguese.
Plus, the advice is all practical and sensible. We might, in ordinary times, think that practical and sensible is boring, but I know it’s something I’m craving at the moment. And I’m also craving information that cuts through all the overwhelming noise and tells me exactly what I need to know.
This site does that.
Massive, massive kudos to JDRF and Beyond Type 1 for getting this initiative up and running. And well done to all the organisations who have happily supported and shared it. This isn’t about ownership and needing to be the holders of all information. It’s about ensuring people with diabetes have access to what we need to know, and what can help and support us. That’s only a good thing, right?
Click on the image below to be taken straight to the site. And stay safe. That’s really what we all want and are hoping for.
DISCLOSURE
I am employed by Diabetes Australia. I am on the Beyond Type 1 Leadership Council.
Until about three weeks ago, I’d never seen the words ‘social’ and ‘distancing’ in the same sentence. And then, suddenly, we were all being urged to practise this new form of keeping away from people.
What became apparent very quickly, however, was that social distancing could very easily lead to social isolation and that is not what the aim of keeping away from others was all about. Rather, it was about being physically distant from others. No more physical hugging, or cheek kissing. No more pats on the back or hand shaking.
But stopping physical contact doesn’t mean becoming disconnected to people. In fact, if there was ever a time that we need to feel connected to people, it’s now. And for me, I have never needed my diabetes tribe more. I think that a number of others might just be in the same boat.
I can’t begin to count the number of times I’ve spoken or written about how much I need my friends living with diabetes to help support my daily life with diabetes, or how they are an essential part of my diabetes management tool kit. In fact, I use this tweet so frequently when I am taking about diabetes peer support because it perfectly illustrates just how essential it is to me.
At the moment, as were locked in our homes, maintaining connections to others is far more difficult. My sister has just returned to Melbourne after over a year living on the west coast and apart from sitting in her garden while she stood at her front door, I’ve not seen been able to welcome her home. I’ve not hugged my parents for weeks, again seeing them only from out the front of their house as they stood on their veranda.
But when it comes to our diabetes peers, I’ve found it a little easier. Our DOC lives over the interwebs. We are physically distant pretty much all the time because most of the people that I spend my time talking to are literally in another country! I may not get to see my friends at conferences and meetings much in coming months, but that hasn’t stopped the messages and photos and videos and video calls.
Each night, before I turn my light out, I message friends to check in to see how they are. It takes nothing to send a quick message but the reassurance that there are others in the same boat, feeling the same fears and frustrations seems to calm and alleviate some of my stresses. And when I wake up there are always messages from friends who were awake while I slept checking back in on me. There are group chats with discussions that range from the incredibly serious to the (thankfully and much needed) absurd. Memes fly around and eyes are virtually rolled at some of what we are seeing online. And sometimes, but only sometimes, we talk diabetes…
I know that pretty much everyone around the world right now has some sort of concerns about COVID-19. Diabetes adds extra to that (because diabetes is a shit and just makes everything more difficult!). And that means that we want to unite with those who understand the extra bit of stress or pressure or anxiety. Find your tribe. And love them so, so hard. (Just do it from a distance at the moment….)





 It’s great that a number of PWD already know that they will be part of ATTD this year, attending satellite events run by different device and drug companies. Some are on the program and some will be there through other opportunities and work.
It’s great that a number of PWD already know that they will be part of ATTD this year, attending satellite events run by different device and drug companies. Some are on the program and some will be there through other opportunities and work.







