You are currently browsing the category archive for the ‘Communication’ category.
It’s Drop the Jargon Day. Here’s one I prepared earlier about this very topic.
So today, I am taking extra care about the words I use and the things I say and write when talking diabetes.
I know I am guilty of being very lingo-istic at times. I read through this blog and see the jargon sprinkled through posts, abbreviations and slang terms littered everywhere. (Huge thanks to someone who commented on one of my posts last week about how I need to not use anagrams so much!)
I catch myself in meetings using shorthand that makes sense to me, and correct myself by explaining terms may be like a second language to those of us required to speak it fluently, but a foreign language to those who don’t.
So today, I am going to use pictures to illustrate this issue. Because a picture tells a thousand words. And a cartoonist is far more amusing that I could ever hope to be! (Click on images for source.)
Take the pledge to Drop the Jargon here.
Today, I just want to follow up a little about one of the points I wrote about yesterday in my post about the event I attended on Tuesday evening about diabetes-related foot complications, specifically this point made my A/Prof Ramon Varcoe:
He explored how we make people with diabetes know this technique for saving limbs is available, and said that it is really, really important to inform PWD about it so that they can ASK for it and not just accept a diagnosis of requiring an amputation. He said that this was the group that could really drive change here, by demanding that they have the best treatment possible.
This had me thinking long and hard. I agree with A/Prof Varcoe here, but that is not really a surprise. I am so much about consumer-led healthcare, that I dream about it (sad, but true).
Mostly, I thought about it in context of my own diabetes care and how it has happened that I am such a DTech nerd. I decided after about two years of living with diabetes that I wanted to use an insulin pump. I really just could not get the hang of the MDI situation I had been put on at diagnosis and was the living embodiment of why Protophane was referred to as Protopain.
I went to an information session and heard a women speaking about how much she loved using an insulin pump and what a difference it had made for her quality of life. Afterwards, I spoke with her and by the end of our chat, was convinced. I wanted one of those! (Impressionable little thing, aren’t I? #MarketersDream) This woman would become my pump trainer and the only diabetes educator I have ever seen.
At my next endo appointment, I marched in with the research I had done, the questions I needed answered and an expectation that by the end of the consultation, I would leave with details of how and when and where I would be getting my pump. Ha, the naivety!
My endo was absolutely not keen for me to take the pump road, ‘You’ve not had diabetes long enough,’ he told me, which confused me no end, because it already felt like a lifetime. ‘I think we should talk about this again after you’ve had diabetes for about 5 years. Yes?’
Well, no. That was the last time I saw him. I spent the next six months endo shopping until I found one that (I was promised) would agree to helping me on a way to a pump. I walked in and made it very clear why I was there and he nodded straight away. ‘Yep – we can do that,’ and picked up the phone. And about three months later, I was a pumper. This particular endo and I parted ways not long after because I needed someone who was far more expert in the diabetes and pregnancy track I wanted to embark, but I have always been grateful that I found him and his open attitude to diabetes technology.
When CGM was launched into Australia, I spoke to my diabetes educator and asked her to fill in the required paperwork to get me sensing. She sent the form off the day we spoke.
And the same has happened when I have wanted to change or upgrade diabetes devices.
What I am trying to say is that this has all been led by me. So when A/Prof Varcoe spoke about the importance and value of connecting with PWD and telling them about these new vascular procedures to save limbs and prevent major amputations, it made perfect sense. He urged that we needed PWD to be the ones who, if told they needed to have an amputation, spoke up and asked for a second or third opinion, specifically asking about the very procedure he had just discussed.
This ground swell of action is what causes change, but we need to know exactly what to ask for. It’s far more effective to ask the question ‘Can my artery be revascularised? I understand there is surgery than can do that and may prevent the need for a major amputation.’ rather than just ‘Is there nothing more than can be done?’
So many of the people with diabetes I know are using particular drugs or devices because they have asked for them – not because they were recommended or suggested by their HCP. And this is why PWD need to have all the information. This is why device companies should be going straight to the consumer to share information, not expecting it to happen through HCPs. (I know that there has been discomfort from some HCPs at Abbott’s direct to consumer promotion of Libre – and the fact that PWD can order themselves without needing to see a HCP, but why would that be the case?)
But it is more than just making sure the information is there for PWD to know and see. It is a complete and utter reshaping of a system that a lot of times actually isn’t about empowerment. There are still too many ‘old school’, patriarchal attitudes that dictate care choices to the PWD instead of accepting and encouraging us to lead the way for our own care. I think things are changing, but I also think they are changing far too slowly.
Apparently, I went to Munich. I was away for 6 days, and 60 hours of those days were spent in transit. I believe that, (as I deal with jet lag, hypoglycaemia, and mainlining caffeine), it is fair and accurate to say that I am too old for this shit.
I am also incapable of forming paragraphs. But dot points are fun! Here are some observations and a few silly thoughts from last week. (I’ll write some sensible things when my brain is back in the same country as the rest of me.)
- I am told by people Munich is a lovely city. I will have to take these people’s word for it, ‘cause I saw very little of the city.
- I did not buy a dirndl and for this, I will be eternally sorry. As will my husband.
- The EASD conference itself was, as predicted, very rats and mice-y. I sat in a number of sessions and wished I was a mouse (while wishing my diabetes away). Alas, I am not a mouse. And I still have diabetes. Damn.
- I did not get sick of laughing at the fact that one of the halls at ICM Messe München is called Langerhan Hall. Also, I did not get sick of saying ‘I wonder if my islet cells are in there’ – to everyone within earshot. Even if I didn’t know them.
- Obviously, Grumps was not as amused by this as me.

- As was the case at ADA, my arm is more recognisable and famous than me. A barista at one of the exhibition hall stands said, as making me a decent coffee, ‘Oh – I know you. I saw your arm the other day near the station.’ I am a walking billboard for Rockadex! (I am not sponsored by Rockadex and purchase my own patches.)
- Dr Kevin Lee from Queensland is a tweeting machine! In fact, I think the thing I was proudest of at EASD was seeing him tweet! (Actually, probably should say that Professor Mark Cooper’s giving the Claude Bernard Lecture was also a moment of national pride, but Kevin’s tweeting was on another level!)

- One of my favourite talks was about diabetes, cardiac health and exercise (go on, laugh….), but that was mostly because presenter Dr Nikolaus Marx, finished up with a discussion about passive exercise and cardiovascular events during the World Cup. If you were in the room, it was me who cheered when he mentioned the increase of cardiac events after Italy beat Germany. (#VivaItalia!). For clarification, I was cheering at Gli Azzuri’s victory, not the number of Germans having heart attacks. (By the way, this was a real study. Published here.)
- A HUGE shout out to these three women. AADE presidents elect, past and present, Nancy D’Hondt, Deb Greenwood and Hope Warsaw are absolute advocates for and champions of people with daibetes, and peer support. This is them at the docday blogger and advocate event. This level of commitment by HCPs to consumer engagement is enlightening, and a lot could be learnt from their example here. Thank you. Thank you. Thank you!

- It was wonderful to see quite a lot of discussion about AP. Anytime someone wants to actually get these into market and into the hands of people with diabetes, that would be just great! Thank you.
- I may have screamed a little when I wandered through the Association Village to the excellent historical display of diabetes by the German diabetes Association. Terrifying might be the word for these needles. I said a little prayer of thanks to the diabetes angels for modern day tech, and for being diagnosed in 1998.

- I need to take a break from twitter. This was the state of play when I said good bye to the conference.

And finally, a word about language, because I am unable to attend a conference and not talk and write about it. (I think it’s actually become a law somewhere.) This probably deserves a post of its own and that may happen, but here we go anyway.
This is the fifth EASD conference I have attended, and going in, I know that it is going to be challenging, language-wise. There often appears to be very little consideration that there could be PWD in the room listening in to how HCPs are speaking of us. In the opening ceremony, I tweeted this at EASD president, Professor Juleen Zierath:

I was a little disappointed at Professor Mark Cooper’s constant use of ‘diabetic’, but it was by no means any more than most of the other speakers. I suppose I just hold Australian speakers to higher account given the work we have been doing here around language and diabetes.
This tweet generated quite a lot of discussion, and came about after I was exhausted and annoyed and mostly frustrated by the way speakers were referring to people with diabetes.
 Perhaps the best response was from Nick Oliver:
Perhaps the best response was from Nick Oliver:

Here’s the thing – and it is something I spoke about during my talk at the DOCDAY event. Language DOES matter. We all know that. It’s completely and utterly disingenuous to say it doesn’t. For some people, it doesn’t bother them and that’s terrific. For others, though, it really does. So why would anyone do something that may offend when it is so easy to avoid that?
DISCLOSE DISCLOSE DISCLOSE
My (economy fare) flights and accommodation expenses were covered by AMSL and J&J. I was attending the EASD conference mainly to attend the J&J DOC exchange meeting which I was involved in preparing and presenting. No one ever expects me to write anything. These are my words and observations only. (And seriously, have you seen what I have just written? No one wants to be associated with that!)
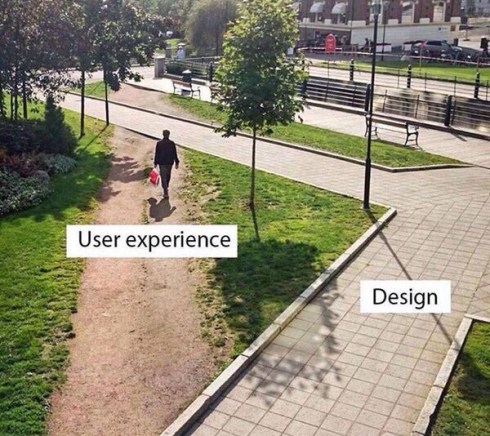
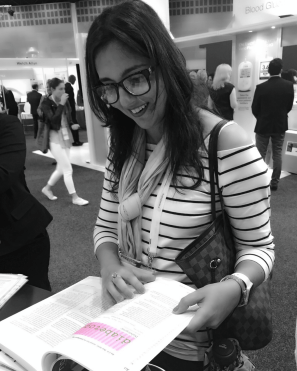
This photo* sums up why I do what I do, and why many people think I sound like a broken record, with a vocabulary of a mere seven words. Specifically, these seven words: ‘Have you spoken to people with diabetes?’
Because so often, the answer is ‘No’. Or ‘No – we’ll be doing that after we have had some meetings.‘ Or ‘Yes – we spoke to you‘ at which point I remind them that I pointed out when they did indeed speak to me that they should find other people with diabetes to speak with. Because I am but one person and speak for no one other than me. (Or, perhaps, another woman in her 40s who loves Nutella, boots, coffee, lives in inner-Melbourne, waves her hands around madly while speaking reallyreallyreallyreally fast, can recite Marx Bros movies from start to end, has what some would call an irrational fear of birds (and butterflies), can sing (badly) pretty much any song from the 1980s, has over 25 striped t-shirts in her cupboard and is battling an eleven year old daughter who has decided that she too loves stripes and wants to borrow all her mother’s clothes.)
Most people are not like that. (Fortunately.)
Anyway, this picture also demonstrates that those who have the privilege of designing services, activities, programs, settings for people with diabetes often miss the point – perhaps not by much, but nonetheless, they miss it. It’s usually because they forgot to ask us, or asked as too late, or didn’t keep coming back and asking and checking in. And then, when we don’t use what they design, we are branded ‘non-compliant’ or ‘disengaged‘ or ‘not interested in our health’, when the truth of the matter is that their design (without our input) just doesn’t fit our needs.
I have given so many talks and written so many pieces about this. But perhaps all I need is this on a t-shirt, tattooed to my arm (forehead?) and on the back of my business cards. Don’t design before speaking to the user. It’s actually really easy!
(*I don’t know the source of this photo, but if anyone does, please let me know so I can credit appropriately.)
There is a dance I do with diabetes each and every day. I praise, celebrate and highlight the good; I avoid, shut out and ignore the bad. The things that scare me are pushed away – as deep as they can go. When they threaten to rise to the surface, I do the equivalent of sticking my fingers in my ears and start chanting ‘la, la, la’ so they recede to where they belong. Out of sight. Out of mind.
I’ve done this for as long as I’ve had diabetes. From day one, I pushed away the ugly and scary images of diabetes complications. I conveniently ignored the warnings and threats. Obviously. Because no one wants to be scared or warned or threatened the day they find out they have a life-long chronic health condition. Or ever.
I am scared. Diabetes scares me a lot. It always has, but for some reason, it is more at the moment. I don’t know why. Nothing has changed. There has not been a frightening experience or a noticeable change in anything. But as days and weeks and months and years as a person with diabetes gets crossed off some imaginary calendar, I am suddenly feeling that it is a countdown to where the really difficult things start.
I worry about what each passing hour is doing to my body and to my mind. If I’m being particularly forgetful, I wonder if it is because my head is so full of diabetes considerations that there is no room for a synonym for fear (dread, anxiety, terror, dismay alarm….) or recalling what day my kid has library each week.
But thinking about it more, I think the fear comes from the lies we are sold about our diabetes. I was promised the day I was diagnosed by a lovely, but most likely completely out of touch doctor, that diabetes is a matter of maths and that if you do the equations properly, it can be easily controlled.
Diabetes can’t be controlled, and with each moment of failure – and there are many and they are constant – I have feared the consequences. And I fear diabetes. With each missed calculation or out-of-range number or confusion about how the hell this thing really works, I see failure. And fear.
Diabetes is not a matter of maths, and the idea that I can control it results in a constant state of high alert as I pretend to be a body part that, when working, is pretty damn perfect. I am not perfect. In any way. And neither is the way I manage my diabetes. It’s messed up. And I’m messed up about it.
And now, as always, there are the fears. And they seem bigger and bolder all the time. I fear diabetes-related complications – long- and short-term. I fear losing the ability to take care of myself and care for others. I fear diabetes becoming so intrusive that I am unable to do anything else. And I fear diabetes becoming the first, last and only thing others think about when they see me. Perhaps most of all, I fear diabetes becoming the first, last and only thing I think about when I see me…
I wonder just how differently I would feel about diabetes – the known and unknown – if I was told at diagnosis that I would get this wrong more times than I got it right. And that was perfectly okay, understandable and acceptable. I wonder how much less significant the feelings of failure would be. And how much more in check my fears would be.

9 March, 1998. 37 days before diagnosis.
I had a call the other day from one of my favourite diabetes HCPs who is writing about diabetes and female sexual health. I wanted to shout ‘Halle-fucking-luiah!’ but didn’t because I am polite and never swear.
Anyway. The reason I was so excited to hear this is because when it comes to diabetes and sex, women rarely get a look in. Let me reframe that. When it comes to information about diabetes and sexual health, women rarely get a look in. (Hopefully women with diabetes who are wanting sex are getting plenty of looks in…so to speak…Yeah, this is not going to be awkward at all, is it?)
When talking about the complications of diabetes, erectile dysfunction*** frequently is mentioned. It is actually one of the things that often get men to the doctor because, well, because…erectile dysfunction. There is information about it and it is a well acknowledged complication of diabetes in men.
But women also report problems with sexual function, yet there is very little information about it and it is spoken about very, very rarely. Or, when it is, it’s discussed around changes in sexual function relating to menopause, which may be an issue for all women – diabetes or not. I guess the thinking is that ‘this is when it is likely to be a problem, so let’s talk about it now’, which doesn’t really help those who may have concerns with sex and sexual function earlier than menopause.
So today, let’s talk about women’s health and diabetes – all of it, including the sex stuff.
(For the record, there is no kissing and telling in this piece. There will be no personal sharing of sex stories. This is for everyone’s benefit! Plus, I learnt that it is not cool to discuss my sex life in a public forum after I once mentioned in a talk to a group of first year med students that I hypo pretty much every time after sex, and then made some silly comment about it being because my partner was so good in bed. This would have been fine if it all stayed in the room. The next night, when out for dinner, a group of Uni students came up to me and told me that they had been at my talk the day before and it was great. Then they looked at my husband who was innocently eating a plate of pasta and one of them said ‘Well done, mate.’ I was mortified. Anyway, let’s move on…)
So, what is out there now for women who want some information about diabetes and sex? Well, while working at Diabetes Victoria we developed a nifty and gorgeous looking booklet which talks about contraception choices. It’s called Sexual Health and Contraceptive Choices for Young Women with Type 1 Diabetes, and I can’t for the life of me find it online, but if you can get a copy, it’s terrific!
There are also some great Australian resources available on diabetes and pregnancy – both for women with type 1 and type 2 diabetes – which provide information about pre-conception planning as well as what happens after conception, during the pregnancy, during delivery and post-partem.
There is some (limited) information about diabetes and breastfeeding. (So wish there had been more eleven years ago because, seriously, I bumbled my way through for almost 24 months and it was horrid at times, diabetes-wise…)
But where is the stuff about everyday diabetes and women’s health and sex – not necessary tied up with trying to get pregnant. (We’ll ignore the ‘tied up’ comment there, okay?)
On the day I was diagnosed, a lovely diabetes educator told me that sex is exercise. Exercise often causes hypos. Hypos are not fun. Not fun kills the sex stuff. Moral of story – keep jelly beans beside bed. I was terrified that I was going to pass out during sex and that it was going to be unpleasant for everyone involved. (Not that there would be a cast of thousands…)
Yawn – it was boring information and it made me think that in future, sex was going to very unsexy. What I wanted to hear was ‘you absolutely can still have sex and, if you want to, you absolutely should. There are some things you might want to consider such as the possibility of going low… I’m talking about your blood sugar, get your mind out of the gutter, Renza, and wipe that smile off your face… so Nutella body paint is a good idea.’
Now that would have made me smile, think of Nutella as a medical necessity and therefore how diabetes now justified me keeping a jar of Nutella by the bed. And on the kitchen table. In the bathroom… basically anywhere! As an emergency contingency, of course.
No one ever spoke to me about what orgasms may do to my BGL. Nor was I told much (in fact, anything!) about how high BGLs might impact on sexual function.
And then there is the minefield that is body image and diabetes, and thinking about how we feel about ourselves and its impact on how much we want to have sex. Or how it makes us feel when we are actually having sex.
Plus, the visible signs of out so-called invisible illness impact on how we feel about undressing in front of someone. I have scars all over my abdomen and hips from heeling pump sites. There is usually a CGM sensor strapped to my arm and a pump cannula in my tummy or hip. There are dregs of tape from old sensors and sites and sometimes tiny bruises. There are tubes and a little vibrating machine (pump, people…I’m talking about my pump).
All of these things point to the fact that I am not perfect and that my body is not perfect and that I need devices and drugs to keep me ticking along. This makes me feel crap at times, wonder what my partner is thinking and want to hide all the reminders that I am not a perfect woman away. This sucks even in my situation where I am married and have had the same partner since diagnosis. Add to that the idea of exposing and explaining all this to someone new and you bet that will impact on how one feels about one’s body and the very idea of sex.
I remember being warned a million times about how women with diabetes MUST PLAN PREGNANCY. And this is excellent advice. However, it made me so terrified of getting pregnant with a sub-perfect A1c. I learnt that fear is an absolute libido-killer. Even when pregnancy would have been welcomed, I was terrified to fall pregnant before I’d been given the green light by my endo.
…which for a while made me feel like there were more than just the two of us in the room trying to make a baby when we were…well…trying to make a baby.
My diabetes loomed overhead, and every moment, I was petrified of my BGL. I started pondering ridiculous things like ‘If I conceive right now and my BGL is not in range, what will that mean? Is it possible that my baby may not have eyelashes if that happens?’ Way to go being drawn out of the moment and into a weird space of imagining babies without eyelashes and how they would hate me forever and ever, and never be able to wear mascara.
So, who do you talk about if you want to have a chat about diabetes and sex? I have never ever been asked about my sexual health from any of my healthcare professionals. Of course there have been discussions about contraception and pregnancy planning and actually being pregnant. But no one has ever said ‘Does your diabetes in any way impact on how you feel about sex? Or do you think diabetes might impact on actually having sex?’
For the record, (and this is a personal bit), I did find that my attitude to sex changed after I was diagnosed. I am sure that was connected to how I felt about my body, so there was some psychological stuff I needed (and continue) to work through, but there was also a noticeable difference in actual function and how I felt. I couldn’t find any information about it, so naturally, thought it was just me.
Of course, it wasn’t. And as soon as I spoke to a group of women the same age as me who were all experiencing similar things, I felt heaps better. But it took me a long time to find those women and feel comfortable speaking about it (yay for prosecco!).
I don’t really have any answers in this, but I wanted to write to start a discussion. I know of many women who say that they believe diabetes has an impact on their sex life – both physically and emotionally. Also, I have come to understand that if it is an issue for one, it is usually an issue for many. Anything anyone want to share? Feel free to do so – anonymously if easier.
***LANGUAGE DIGRESSION
Erectile DYSFUNCTION? Can we please come up with a different term for this? Dysfunction sounds like failure – or at least like a penis has failed. It has not.
Last night, I was the ‘here’s one we prepared earlier’ on a panel discussing CGM technology. The audience was all healthcare professionals – mostly DEs, but some dietitians, RNs and also a GP-in-training (so much yay to him for coming along!).
I love being in the room for these events! I wrote about my last experience giving the same talk here. I cannot speak highly enough of the two experts on the panel last night. Dr Peter Goss – who spoke at the last one of these events – is what I would call a disrupter in the diabetes healthcare space and, honestly, all the power to him. He may ruffle some feathers with his sometimes unorthodox approach, but it is undeniable that he is a champion for kids and teens (and young adults) with type 1 diabetes. Also on the panel was A/Professor David O’Neal who is best described as a truly awesome endo (I have heard that from every single person I know who sees him as their endo) and an absolutely brilliant mind. His expertise in diabetes tech is second to none and he is genuinely interested in how the technology can safely, efficiently and effectively be incorporated into the lives of people living with diabetes.
I know that all sounds rather effusive. But I need to point out that they are remarkable. And that they are the sorts of HCPs you want on your side if you are a person with diabetes.
Because now I am going to talk about language and why I pulled them up a little bit after we all did our presentations and sat on the stage ready to answer questions from the audience.
As happens frequently when I am in the room with a group of healthcare professionals, the conversation turned to language. Okay, I made that happen. In fact, the words I used were ‘I’m going to hijack this conversation because we really need to talk about language here.’
One of my biggest pet peeves is the jokey, and somewhat snide, comments made about people with diabetes making up numbers in their diabetes log books. Because, it’s not a joke. It’s not something for HCPs to roll their eyes over and dismiss as ‘non-compliant’ behaviour.
The word that was used for PWD who make up numbers in their books was ‘fakers’. I cringed the moment I heard the word. And cringed even more at the audience’s response – laughter, heads shaking from side to side and knowing looks. I looked around the room and knew that we would be talking about this later on in the evening!
As I pointed out when the panel was seated on the stage, I absolutely did this. And I was incredibly good at it – different coloured pens, splotches of blood on the pages, dog-eared corners of the book. Once, I even splattered a few drops of juice, because on that particular page, I was having a lot of lows and I thought the juice would make it look more authentic.
Now, let’s all just remember for a moment that I was diagnosed as an adult. This wasn’t insolent teenager behaviour. This was a woman in her mid-twenties who was terrified of disappointing and being judged by the HCP to whom she would be handing the grotty book and its made up numbers.
I told the room my story of this last night and there was laughter – because the way I spoke about it was amusing. It was a cheeky anecdote. But at the time, it wasn’t funny. I was scared, I hated checking my BGL, I was paralysed by numbers that didn’t make sense and I didn’t know what to do about it. So I lied. Of course my HCPs knew that. And I knew my HCP knew.
But the question is about WHY people do this. The discussion needs to stop being about diabetes at that point, because really, managing BGLs and most other diabetes tasks is not the issue here. The issue is distress, anxiety, fear. And, in my case, I felt desperate.
One of the panellists made the point that the reason that he brought it up was because HCPs need to know what to do when someone is ‘faking’ their numbers. He’s right. I completely agree. And then there needs to be understanding of how to approach it, which is likely to be different with each PWD.
For me, it took until I found a HCP who I felt I could trust – one who wouldn’t judge the numbers that were out of range (which one HCP always circled in red pen, making me feel even more like a delinquent adolescent) – and was interested in knowing what was stopping me from feeling able to check my BGL.
When we worked through that, I was better equipped to not only regularly check my BGL, but also to deal with the numbers and act upon them. I came to understand that a number was nothing more than a piece of information that I could use to make a treatment decision – not an indication of me being a good or bad person.
Language does matter. And words count for a lot. Using the word ‘faker’ in this context is loaded with judgement and accusation, and even if that is not the intention, it made me – a person with diabetes – feel very uncomfortable. But mostly, it fails to consider the real problem at hand which is not that a PWD is making up numbers in a book. It is why they feel the need to do that.




 It’s about words, because language matters and sticks with us forever.
It’s about words, because language matters and sticks with us forever.