You are currently browsing the category archive for the ‘Wellbeing’ category.
When I was in my teens and twenties, I was, just as many women are, dismayed with the way I looked, and susceptible to the claims of beauty products that promised I could be thinner, more toned, more beautiful, smoother, more attractive, more <insert whichever part of me obviously needed improving>.
Of course, all of the things I was desperate to change and refine were measures of my worth, right? Because if I was thinner, more toned, more beautiful, smoother, more attractive, more <insert required improvement> that would make me a better person. Right? Of course.
I didn’t look like one of the supermodels (not just models, mind; these ones were super) that were everywhere I looked. At the time, I was spending all my energies being a flute player, but even the classical musical world wasn’t spared the attention to how women should look, with Jane Rutter suddenly appearing wrapped in nothing more than a bedsheet and a sultry look (impressive with a flute shoved against her bottom lip, while playing Debussy). ‘Great’, I thought. ‘Now not only do I have to look like a fucking model. I have to do it while playing flute. Naked.’
The feelings of inadequacy were strong and I know I spent far too much time desperately wishing I looked different. I probably spent too much money on products that promised to make that happen. And delivered nothing.
When I was twenty-one, someone gave me a copy of Kaz Cooke’s fabulous book Real Gorgeous. I can’t remember who it was, but suspect it was my mother. I read it in one sitting. I already knew of Kaz Cooke (from her brilliant ‘Keep Yourself Nice’ column in the weekend papers), but this book was a revelation. She laid bare all the sneaky tips and tricks and lies the beauty industry used to expose our insecurities, feel as though we needed to be different and, subsequently, buy their products. Of course, I already knew what she was saying. There was nothing in there that, when I had a moment of rational thinking, I didn’t already understand. But to have it set out so practically and emphatically was just what I needed to get over the idea that I needed to look and be different to how I was.
I actually saw Kaz at Marios over the weekend and stopped her she walked past me. I introduced myself and the kid (who was so horrified and embarrassed that she looked as though she wished the ground would swallow her up), and thanked her for all her books, but especially Real Gorgeous. ‘It saved me, in some ways.’ I told her.
And it did. It stopped the self-doubt. And it made me confident enough to admit to myself that I was more than enough. Just the way I was. And that nothing about the way I looked needed improving. (Thankfully, this was before I tried any naked flute playing. At least, any in public…)
As it turns out, I struggled with the same insecurities and feelings of inadequacy and self-doubt when it came to being diagnosed with diabetes. I think it is only in recent years that I have come to understand that the constant second guessing about being good enough achieves nothing other than increasing my anxieties and contributing to burn out.
With time, I came to apply the same cynical filters to diabetes product advertising as I now had permanently in place when looking at health and beauty advertising. In the same way that not every woman looks like Cindy Crawford, not every blood glucose check will be 4.8mmol/l.

‘Real Gorgeous’ wisdom on the left. Real diabetes on the right.
One of the most damaging things that we can do is compare ourselves to others. Because when we do, we often fall short. Our A1c may be higher, our time in range lower, our technology not as advanced, our healthcare professionals not the ones on the TV or on conference stages.
Being around and sharing with others living with diabetes is wonderful (here are twenty reasons why) but it can be damaging if the only thing you are doing is using them as a yardstick for your own diabetes.
It took me many years to stop feeling that I needed to ‘keep up’ with my diabetes peers, or that my diabetes needed to look like someone else’s diabetes. While I may try to align myself with others who have similar ideas about diabetes, I do it on my own terms, using and doing the things that work best for me.
The way I have adopted DIYAPS is not the same as many others. I call it ‘Loop Lite’, using just the absolute basics, without any of the add-ons. I don’t produce pages of graphs to analyse, because that’s not what I need. But what I do is perfect for me.
The same goes for finding the way to an eating plan that works for me. While learning about the details of LCHF, I refused to go ‘all in’ as many seem to. I adapted it for the way I live.
The way I do diabetes and the way my diabetes behaves is enough. It is right for me. It is my Real Diabetes.
Today, I have a brand new copy of Real Gorgeous on my desk, all wrapped up. It’s a gift for the kidlet who is already a huge Kaz Cooke fan (she has had Girls Stuff on her shelf for a few years now). She already has a very healthy filter when it comes to beauty advertising, but I know that it is possible that she will be susceptible to the same feelings of self-doubt that I was.
I want her to know she is enough. So very much more than enough. We all are.
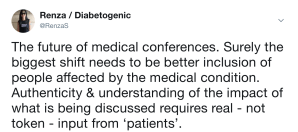
There is an indescribable feeling I have following a diabetes conference. Swirled in amongst the exhaustion, information overload, jet lag (because conferences are always in ridiculous time zones that are not AET), and memories, I come back galvanised in a way that can only happen when spending time with those in my tribe: others living with diabetes.

I returned from three days in Vienna bone-achingly exhausted. After being reunited with my family and not being able to stop hugging them, a few days of not-great-but-okay sleep and bucket-loads of Melbourne coffee under my belt, and time to process and write about what I learnt, I find myself recalibrated and ready for what’s next.
The hours of travel is a memory, the conference sits comfortably alongside all the others I’ve been too, my conference name badge is hanging in my office with all the others, and I’ve plans already underway from successful meetings.
In a lot of ways, the status quo has been restored and I am back to my real life after a few days of conference life.

But what is not the same is the level of vitality I now have, my veins pounding with the vigour that comes only from spending time with the people who are working to and for the same things because they get it at a personal level that is only apparent to those of us whose very DNA is affected by this condition.
I came to realise a few years ago that I have an invisible jar in my mind, and how empty or full that jar is depends on the time I’ve spent with likeminded diabetes friends. When the jar is nearing empty, I find it difficult to focus my energies on the advocacy and support issues that often are front and centre of my mind. I feel myself flailing and falling short because I don’t have the support of those I need to boost me up.

Of course, I am lucky enough to have others with diabetes around me even when I am in Melbourne (hello neighbour!), but it is those I see at these sorts of conferences – the ones whose minds and hearts are full of similar ideas, similar frustrations and find similar reasons to celebrate– that fill that jar right up. It is when I can simply turn to someone because they are sitting right there, have an animated conversation and high five each other with our enthusiasm that I feel capable and able to take on the world.
Those people who share my pancreatically-challenged existence, who breathe the same health condition, and struggle, celebrate and despair in similar ways to me, are the ones who fill up the jar ways to sustain me until the next time. My motivation is high, the momentum fast, my mind is working overtime. And my jar is overflowing right now with those people who may have beta cells that don’t work, but they make up for it in ways you couldn’t even begin to imagine.

Tine – who inspires me every time we speak.
It’s not really a great day in diabetes with news all over my SoMe feeds about a study published in Diabetologia which links high glucose levels with dementia, and a report from the Baker Heart and Diabetes Institute showing Aussies with type 2 diabetes are twice as likely to suffer sudden cardiac death.
Perspective is really important on days like today. I’m not in any way wanting to minimise the significance of the these reports – obviously we should take them seriously. But equally, I think we also need to find some positives in the diabetes space and remember that it is not all dire and critical.
Diabetes is serious and anyone who thinks otherwise doesn’t know diabetes. This weekend, a true giant in Australian diabetes died. Hal Breidahl was a pioneer who co-founded the Australian Diabetes Society. In a piece he wrote back in 1980 (and the language reflects that it was written in 1980!!!) about what people with diabetes want to know he states:
All diabetes is severe – unless adequately controlled. Patients often want to know ‘how bad is my diabetes?’ or ‘how severe is the condition?’ or ‘how high is the blood sugar?’ The notion that ‘I’ve only got a touch of sugar’ or ‘I only have mild diabetes’ should not be allowed to remain…
We get it. Diabetes is serious. Nasty things happen. We know it.
But I want to add to this. There is – there has to be – more to diabetes than the negative stories that make the news. Because in amongst those stories there are these things to remember, and I seek them out each day:
- Diabetes is serious, but it is also the condition I need to live with and find some semblance of balance as I work out how to fit it into my life.
- I need more than just the negatives, or bad news highlights. Because not offering the things I can do to live as best I can does nothing for my mental health – or for my diabetes health.
- Attention grabbing headlines that only tell part of the story do nothing to make me believe that I will be able to live well with diabetes. Also, ‘live well’ means different things to different people and it’s a moveable feast, but I know that the idea that we need to be complications-free to be living well is a flawed and dangerous idea.
- There is a lot of positive research about diabetes and we need to know about that too. Like this which reports people with type 1 diabetes are living longer.
- There is an undeniable truth that reading over and over and over again that diabetes is going to increase my risk of <insert whatever you bloody well feel like> is exhausting. I feel as though I have been kicked in the gut every time it happens even though I know that I am living the best diabetes life I possibly can.
- While diabetes may increase the risk of all sorts of things, sometimes it just doesn’t, because sometimes it’s not diabetes. If others could remember that, it would be useful so that any other affliction isn’t automatically lumped in the ‘It’s because you have diabetes’ basket, and not investigated properly.
- If you are talking about the nasty things that diabetes seems to increase the risk of, please acknowledge that the tools we have to live with this condition are not up to the task. Any failure is not mine as a person with diabetes. It is the failure of a body part that decided to not to what it is supposed to. It is a failure of the insulins currently available not being able to act fast enough. It is a failure of monitors not being accurate enough and delivery devices not delivering properly. Please remind people of that when you also mention that out of range glucose levels (AKA diabetes) means that we’re at a higher risk of not-so-great things.
- The bad stuff? It may not happen.
On a day like today when I am reading a lot about the diabetes things I really don’t want to think about, it is especially important for me to find some of that balance and search out the good news. Because otherwise diabetes tips into a really dark place where good self-care becomes almost impossible. There is light in diabetes. And sometimes, we need some help finding it. Sometimes we need to search a little harder to see it. Today is one of those days.
I wrote this post on this day last year and today, when it came up in my TimeHop app reread it and realised it is a good one to consider at the beginning of the year as I’m trying to get myself in order. I’ve made some edits to some of the points due to changes I made last year in the way I manage my diabetes. (The original post can be found here.)
I suppose that I was reminded that being good at diabetes – something I’m afraid I miss the mark on completely quite often – does involve others who sometimes don’t necessarily understand what it is that I really need. And I can’t be annoyed if they don’t intrinsically know what I want and need if I can’t articulate it. This post was my attempt to do just that.
______________
Sometimes, I’m a lousy person with diabetes (PWD). I am thoughtless and unclear about what I need, have ridiculous expectations of others – and myself, and am lazy. But I’m not always like that. And I think I know what I need to do to be better.
Being a better PWD is about being true to myself. It is also about reflecting on exactly what I need and I hope to get it.
- I need to remember that diabetes is not going away
- I need to remember that the here and now is just as important as the future
- I need to remember that I don’t have to like diabetes, but I have to do diabetes
- I need to remember that the diabetes support teams around me really only have my best interest at heart, and to go easy on them when I am feeling crap
- I need to empty my bag of used glucose strips more frequently to stop the strip glitter effect that follows me wherever I go – edit: while this is true, I do have to admit to having far fewer strips in my bag these days due to my rather lax calibration technique
- I need to remember that it is not anyone else’s job to understand what living with my brand of diabetes is all about
- I need to remember that the frustrating and tiresome nature of diabetes is part of the deal
- I need to be better at changing my pump line regularly – edit: even more so now that I am Looping and think about diabetes less than before.
- I need my diabetes tasks to be more meaningful – quit the diabetes ennui and make smarter decisions
- And I need to own those decisions
- I need to see my endocrinologist – edit: actually, this one I managed to nail last year and even have an appointment booked in for a couple of months’ time!
- I need to decide what I want to do with my current diabetes technology. There is nothing new coming onto the market that I want, but what about a DIY project to try something new? #OpenAPS anyone…? – edit: oh yeah. I started Looping….
- Or, I need to work out how to convince the people at TSlim to launch their pump here in Australia – edit: even more relevant now after yesterday’s announcement that Animas is dropping out of the pump market in Australia
- I need to check and adjust my basal rates
- I need to do more reading about LCHF and decide if I want to take a more committed approach or continue with the somewhat half-arsed, but manageable and satisfactory way I’m doing it now – edit: sticking totally to the half-arsed way and happy about it!
- I need to remind myself that my tribe is always there and ask for help when I need it
- I need to make these!
And being a better PWD is knowing what I need from my HCPs and working out how to be clear about it, rather than expecting them to just know. (I forget that Legilimency is not actually something taught at medical school. #HarryPotterDigression)
So, if I was to sit down with my HCPs (or if they were to read my blog), this is what I would say:
- I need you to listen
- I need you to tell me what you need from me as well. Even though this is my diabetes and I am setting the agenda, I do understand that you have some outcomes that you would like to see as well. Talk to me about how they may be relevant to what I am needing and how we can work together to achieve what we both need
- I need you to be open to new ideas and suggestions. My care is driven by me because, quite simply, I know my diabetes best. I was the one who instigated pump therapy, CGM, changes to my diet and all the other things I do to help live with diabetes – edit: And now, I’m the one who instigated Loop and built my own hybrid closed-loop system that has completely revolutionised by diabetes management. In language that you understand, my A1c is the best it’s ever been. Without lows. Again: without lows! Please come on this journey with me…
- I need you to understand that you are but one piece of the puzzle that makes up my diabetes. It is certainly an important piece and the puzzle cannot be completed without you, but there are other pieces that are also important
- I need you to remember that diabetes is not who I am, even though it is the reason you and I have been brought together
- And to that – I need you to understand that I really wish we hadn’t been brought together because I hate living with diabetes – edit: actually, I don’t hate diabetes anymore. Don’t love it. Wish it would piss off, but as I write this, I’m kinda okay with it
- I need you to remember that I set the rules to this diabetes game. And also, that there are no rules to this diabetes game – edit: that may be the smartest thing I have ever written. I’d like it on a t-shirt
- I need you to understand that I feel very fortunate to have you involved in my care. I chose you because you are outstanding at what you, sparked an interest and are able to provide me what I need
- I need you to know that I really want to please you. I know that is not my job – and I know that you don’t expect it – but I genuinely don’t want to disappoint you and I am sorry when I do
- I want you to know that I respect and value your expertise and professionalism
- I need you to know that I hope you respect and value mine too.
And being a better PWD is being clear to my loved ones (who have the unfortunate and unpleasant experience of seeing me all the time – at my diabetes best and my diabetes worst) and helping them understand that:
- I need you to love me
- I need you to nod your heads when I say that diabetes sucks
- I need you to know I don’t need solutions when things are crap. But a back rub, an episode of Gilmore Girls or a trip to Brunetti will definitely make me feel better, even if they don’t actually fix the crapness
- Kid – I need you to stop borrowing my striped clothes. And make me a cup of tea every morning and keep an endless supply of your awesome chocolate brownies available in the kitchen
- Aaron – I like sparkly things and books. And somewhere, there is evidence proving that both these things have a positive impact on my diabetes. In lieu of such evidence, trust and indulge me!
- I need you to know I am sorry I have brought diabetes into our lives
- I need you to know how grateful I am to have you, even when I am grumpy and pissed because I am low, or grumpy and pissed because I am high, or grumpy and pissed because I am me.
- Edit: I need you to keep being the wonderful people you are. Please know that I know I am so lucky to have you supporting me.
This week, for the first time ever, I had no anxiety at all as I prepared for my visit to my endocrinologist. I always feel that I have to put in a disclaimer here, because I make it sound like my endo is a tyrant. She’s not. She is the kindest, loveliest, smartest, most respectful health professional I have ever seen. My anxieties are my own, not a result of the way she communicates with me.
Anyway, now that the disclaimer is done, I walked into her office with a sense of calm. And excitement. It was my first post-Loop appointment. I’d eagerly trotted off for an A1c the week earlier (another first – this diabetes task is usually undertaken with further feelings of dread) and was keenly awaiting the results.
But equally, I didn’t really care what the results were. I knew that I would have an in-range A1c – there was no doubt in my mind of that. I know how much time I am spending in range – and it’s a lot. And I have felt better that I have in a very, very long time.
The eagerness for the appointment was to discuss the new technology that has, quite honestly, revolutionised by diabetes management.
I sat down, she asked how I was. I marvelled – as I always do at the beginning of my appointments with her – how she immediately sets me at ease and sits back while I talk. She listens. I blabber. She never tries to hurry me along, or interrupts my train of thought. I have her full attention (although I do wonder what she must think as my mind goes off on weird, sometimes non-diabetes related tangents.)
And then I asked. ‘So…what’s my A1c? I had it checked last Wednesday.’ She told me and I took in a sharp breath. There it was, sitting firmly and happily in what I have come to consider ‘pregnancy range’. Even though that is no longer relevant to me, it frames the number and means something.
I shrugged a little and I think perhaps she was surprised at my lack of bursting into tears, jumping up and down and/or screaming. I wasn’t surprised. I repeated the number back to her – or maybe it was so I could hear it again. ‘And no hypos.’ I said. ‘And minimal effort.’
I’ve had A1cs in this range before. In fact, I managed to maintain them for months – even years – while trying to get pregnant, and then while pregnant. But the lows! I know that while trying to conceive and during pregnancy, I was hypo for up to 30% of the time. Every. Single. Day.
It was hard work. No CGM meant relying on frequent BGL checks – between 15 and 20 a day. Every. Single. Day. And it meant a bazillion adjustments on my pump, basal checking every fortnight and constantly second guessing myself and the technology. Sure, that A1c was tight, but it was the very definition of hard work!
This A1c was not the result of anywhere near as much effort.
Surely the goal – or at least one of them – of improved diabetes tech solutions has to be about easing the load and burden of the daily tasks of diabetes. I’m not sure that I’ve actually ever truly believed that any device that I have taken on has actually made things easier or lessened the burden. Certainly not when I started pumping – in fact, when I think about it, it added a significant load to my daily management. CGM is useful, but the requirement to calibrate and deal with alarms is time and effort consuming. Libre is perhaps the least onerous of all diabetes technologies, yet the lack of alarms means it’s not the right device for me at this time.
These tools have all been beneficial at different times for different purposes. It is undeniable they help with my diabetes management and help me to achieve the targets I set for myself. But do they make it easier to live with diabetes? Do they take about some of the burden and make me think less about it and do less for it? Probably not.
Loop does. It reduces my effort. It makes me think about my own diabetes less. It provides results that mean I don’t have to take action as often. It takes a lot of the thinking out of every day diabetes.
So let me recap: Loop has delivered the lowest A1c in a long time, I sleep better that I’ve slept in 20 years, I feel better – both physically and emotionally – than I have in forever. And I feel that diabetes is the least intrusive it has ever been.
Basically, being deliberately non-complaint has made me the best PWD I can possibly be.

Oh look! Your phone can now be deliberately non-compliant too, thanks to designer David Burren. Click on the link to buy your own. (Also comes in black and white.)
We can work out how much we fork out to pay for diabetes.
It’s expensive. Of course it is. When I added up the costs earlier this year for a Diabetes Blog Week post, I estimated our family budget takes a hit of about $6,500 (excluding private health insurance) each and every year. That’s a lot of cups of coffee and a lot of pairs of boots.
But if I talk about the financial burden of diabetes alone, I’m selling short just how expensive the condition really is. The dollars I fork out each year are only one part of what it costs me – although it is a lot easier to quantify.
Because, there’s time. So much time.
We sit in waiting rooms, travel to appointments, take time out to make calls to make those appointments, call the pharmacy to order insulin and supplies, visit the pharmacy to collect insulin and supplies. Our prescriptions run out and we have to hastily find a time and way to refill them. We sit on the phone waiting to receive pathology results. We take time out of work time, out of family time, out of social time, out of our own time because diabetes demands it.
And then there is time dedicated to the day-to-day minutiae of ‘doing diabetes’. The time it takes to check our BGLs, or change a pump line, or site a new CGM sensor. Then there is the time to look at data, and act upon it. We lose time to treat lows, treat highs, watch CGM traces, question what to do with random numbers. We build up a sleep debt that never gets repaid, no matter how many early nights or nanna naps we try to sneak in.
It adds up. It all adds up – slowly and deliberately until suddenly we realise just how much time it takes. I tried to give a dollar amount to the time I spend doing diabetes, and stopped when I realised just how terrifying it was. If I was able to dedicate that much more time to paid work, I’d be spending a lot more time in New York each year. And then I got depressed and decided to stop adding up the hours I spend on diabetes.
But still, this is just scraping the surface. The money it costs and the time it takes are significant and must not be underestimated. However, the harder to measure personal costs and emotional burden should not be forgotten either.
I don’t really know how to gauge the extent of those costs. I don’t know how to quantify the psychological impact of diabetes – most of the time I can barely qualify it. But I know it’s significant.
During this month, there are a lot of efforts to try to explain diabetes to those not living with it. JDRF’s T1D Footprint calculator is doing the rounds again, and it’s an effective way to put numbers to just some of the tasks we do to manage our diabetes. I really like they’ve added an extra element to their social media activation: a photo frame with the words ‘T1DYouDon’tSee’ which acknowledges our invisible condition.
Because that’s the thing about diabetes. We can tally up hours and dollars, but measuring the stuff we can’t see is a whole lot harder. And for me, that’s where the real expense in diabetes lies.
It’s not really diabetes awareness time here in Australia. We save that each year for the second week in July and then add an extra spurt of awareness raising on World Diabetes Day. But many of us still decide to jump on the bandwagon of our US friends as they spend the whole of November talking diabetes and giving everything a blue wash.
I always start the month strong, lining up blue clothes and scarves and other accessories to be worn each day. I head off for a blue manicure, regretting it pretty much the minute I walk out of the nail salon. I change my profile picture, and add blue circles to all my photos. I write about every awareness and advocacy activity that comes my way.
By the time 14 November rolls around, I’m already starting to feel exhausted and over the whole thing and by the time my birthday hits in the final few days of the month, I’m ready to slap anyone who wants me to wear blue. All the different initiatives start to roll into one and I can’t remember what I’ve mentioned and what I’ve forgotten to spruik.
So this year I’ve decided to do things a little differently. I knew that I needed to make a change to my usual gung-ho approach when I shared a fun post-a-different-diabetes-photo-every-day Instagram challenge this morning and realised that I was feeling a little ambivilent. I was already feeling the pressure of deciding what to post and didn’t want to commit to posting a diabetes-related photo every day to my socials. So I deleted the post and thought about what I really wanted to achieve this month. And I decided that I want to take a gentle approach to my awareness efforts.
This year, when I get to the end of November, and look back over the month, I’m okay if my SoMe feeds are not a daily reminder of awareness-raising activities. I’m fine with not telling every single person I see that it’s diabetes awareness month and then share one new fact about diabetes for them to commit to memory. I can live with not being sartorially blue or navy or aqua or sapphire for the next thirty days.
Maybe I have some advocacy burn out. Maybe the last couple of weeks of feeling as though I’ve had to defend my treatment decisions have taken a toll.
And yes, I realise how privileged it is to say ‘I don’t want to do diabetes advocacy this month’ when I don’t need to fight for insulin or diabetes supplies. I won’t be abandoning my efforts in this space. (I know that there are some really important access activities coming up in coming weeks and I will be supporting them.)
But I am going to go easy on some of the other things I’m usually all over. And that’s okay. ‘My diabetes; my rules’ extends to how much we want to talk about it. So this year, I’m talking less. I’m not hitching a ride on every bandwagon and I’m taking it easy with the online activism. I’m going less blue and I am absolutely fine with that. T1D will still look like me. (Oh, but I probably will still get a blue manicure. And I’ll probably still regret it.)