You are currently browsing the category archive for the ‘Engagement’ category.
I’ve been working in diabetes organisations for over seventeen years now. When I look back over that time, there are some issues that have been consistent ‘hot topics’.
One of those issues is diabetes in schools.
I have been involved in a number of projects addressing diabetes in schools, starting with the beautiful documentary-like video ‘Diabetes Basics’, and the adaptation of the excellent Diabetes UK schools packs for families of children with diabetes and their schools, firstly in Victoria, and then the subsequent national roll out of this resource. It is called Mastering Diabetes and it still is used today.
It is easy to understand why diabetes and schools is such an important issue. Ensuring that children with diabetes feel safe at school, are able to manage their diabetes in the way that works for them, and are able to fully participate in all school activities is critically important. There is obviously – and necessarily – a lot of emotion tied up in the matter.
But what I have come to know is that, by and large, everyone involved – parents, teachers and school staff – want children and teens with diabetes to be safe in schools and participate in all school and extra-curricular activities just as any other student would. There just seems to be a lot of confusion about rights and responsibilities, which is often the case when there are a number of stakeholders involved.
So, it was great when, just last month, the Federal Government announced six million dollars in funding for a new program to make it easier for teachers to support school children with diabetes, and give parents some peace of mind, knowing that their children will be safe at school.
It will be the first time that Australia has a nationally consistent training program delivered to teachers and school staff at every school with students with type 1 diabetes. The program will cover, (amongst other things), safe administration of insulin, hypo management, and reducing diabetes-related stigma.
This is good news. Great news!
The program is still in development stage and a key part of putting it together is making sure that all involved have a chance to provide input. One of the things I have heard repeatedly over the years from parents is that they feel that they are often left out of conversations about how to best support their child at school.
Parents: now is your chance!
There are workshops being held across the country for parents of primary and secondary aged children. There is also an online consultation for parents here.
Teachers and school staff are also part of this development phase and there are separate workshops being held for this group as well. And there is also an online consultation for for teachers and school staff here.
Now is the time to have your say.
Disappointingly, numbers for workshops has been extraordinarily low – some sessions have had to be cancelled due to low numbers. Considering the constant criticisms I have heard in the past about parents being excluded from discussions about diabetes and schools programs, I’m a little flabbergasted that this is the case.
At the risk of sounding slightly bossy and harrying, I am urging parents of school aged children to please get involved and help shape this important program. You need to show up. You need to register and attend the workshops. And you need to complete the online consultation.
All the details are here. Share them amongst your networks. Encourage parents and teachers of kids with diabetes to have their say. Everyone – everyone!– wants kids with diabetes to feel safe and supported in schools. Help make that happen.

The Diabetes in Schools program is being funded by the Federal Government and will be delivered through the National Diabetes Services Scheme (NDSS). The program is supported by the key national diabetes health professional and consumer organisations in Australia: Diabetes Australia, the Australian Diabetes Educators Association, the Australian Diabetes Society , the Australasian Paediatric Endocrine Group and JDRF Australia.
I work for Diabetes Australia. I have not been asked to write about this program, however as I am always banging the drum about consumer consultation, it more than makes sense that I am encouraging – and pleading – relevant stakeholders to take the opportunity to be a part of the program consultation.
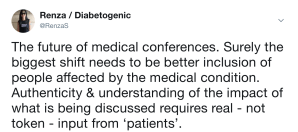
Earlier this week, Professors Jane Speight (ACBRD) and Frans Pouwer (Southern Denmark University) published a blog post on the ACBRD site, with their wrap up of EASD, specifically, the lack of psychosocial sessions at the conference. In the piece, Jane and Frans quite rightly say:
‘Psychology is not an optional extra. If diabetes care is the seat of a three-legged stool, then it is supported by three legs: psychology/education, treatment/technology and complications screening. It seems ironic that so much funding, resource and effort is put into strengthening and promoting the treatment/technology and complications ‘legs’, while the psychology/education ‘leg’ remains short and weak.’
EASD is the largest diabetes meeting on the calendar this year. It draws a truly international audience, with healthcare professionals and researchers from all disciplines. It is possible to speak with endocrinologists, diabetes educators, allied health professionals, general practitioners, psychologists, and researchers from all spheres of the diabetes care spectrum.
And yet, it is undeniable that the conference has a true clinical focus, almost forgetting that diabetes does not only impact specific parts of the body (so, so much about the ‘diabetic foot’!) but the whole person (absolutely not enough on the ‘diabetic mind’!).
I am not for a moment saying that the scientific and clinical elements of diabetes should be removed from a diabetes conference, or that they are not important. But I am saying that by demonstrating ONLY this aspect of diabetes, the picture presented is very, very incomplete.
I have written before that this is a frustration of mine at EASD, along with the continued lack of ‘patient representation’ on the conference program. It astounds me that there are no advocates on the official program, giving the ‘lived experience’ standpoint to what is being discussed. With hours and hours of sessions focusing on complications, how valuable it would be to have a PWD who is living with complications standing up there to give a little perspective to all the science. And a psychologist to speak about how complications affect far more than the part of the body that has become…well, complicated.
I urge the organisers and program committee to step up, and find a way to fill in the gaps and start to present a far fuller and more complete picture of diabetes.
While this would involve including more focus on the behavioural side of diabetes with the relevant professionals on the program, it must also mean including PWD into the program – in a meaningful way. If it is too much of a leap to include PWD alongside HCPs in the scientific program, introduce a Living with Diabetes Stream as the IDF has done in their last four World Congresses. It can be done. It can be done well. (And I say that with full disclosure that I am leading the stream at the 2019 Congress and was deputy lead for the 2017 Congress, and spoke at the 2015 Congress in the LWD stream.)
The thing is, it would actually be very, very simple to include PWD in the EASD program because we are already there. This year in Berlin marked the seventh EASD conference I have been fortunate to attend. I have always gone because of satellite events designed specifically for PWD. Initially, these were run by Johnson & Johnson, and more recently Roche, who has taken the ‘patient engagement’ to a new level, running events with up to seventy bloggers. That’s seventy people who have a story to share about their own diabetes experiences.
And I know that many of those seventy people would want to talk about all aspects of living with diabetes, including the psychosocial impacts.
As a leading annual diabetes meeting, EASD could be better. It ticks a lot of boxes. But it could, quite easily, tick a whole lot more by being far more wholistic in its approach. Focus more on the behavioural side of diabetes. And have PWD front and centre where we belong. After all, we’re the ones all this information and research is meant to be benefitting.
DISCLOSURE
Roche Diabetes Care (Global) covered my (economy) travel and accommodation costs to attend their #DiabetesMeetup Blogger event at #EASD2018 and present at their media event the day before EASD. Roche Diabetes Care also assisted with providing me press registration to attend all areas of the EASD meeting. As always, my agreement to attend their blogger day and participate in their media event does not include any commitment from me, or expectation from them, to write about the company, the events or their products.

With Jane Speight at EASD in Berlin.
The first day of ADC was a hectic one for me. After the busy and generally well-received DIYAPS session, I had a break for lunch and then headed back to the same room as earlier in the day to co-chair a session on co-design.
I quite loved that the idea of this session was included in the program. And even more in love with watching the room fill up as Congress attendees filed in and took their seats. The session was the brainchild of Dr Kirstie Bell, who among other things, is a huge advocate for involving PWD in the program at ADC. She absolutely slayed it with this one!
The planning for the session involved a number of people, including PWD, HCPs and researchers and the aim was to highlight examples of co-design in diabetes and healthcare to help attendees understand that this wasn’t something to be afraid of. I think that sometimes there is an idea that it is just too hard to include everyone because it will mean a lot of coordination and fingers in the pie. But we wanted to show that could be managed effectively.
Another objective was to try to explain the principles of co-design. In this case, it was to underline (and probably italicise and bold) that co-design does not mean showing a finished product to someone and asking for ‘feedback’, with a further point being made that asking for feedback shouldn’t be the aim as that is done when things are already completed. Instead ask for ‘feed in’ the whole way along the process.
If the idea of co-design had a slogan, surely it would be #NothingAboutUsWithoutUs, meaning that the ‘us’ in that phrase need to be the ones driving initiatives – and definitely not being left out. Unfortunately it does seem that in diabetes, often the ‘us’ (i.e. people actually affected by diabetes) are not included in design, instead having others make decisions about what they thinkwe need and want.
And that’s why I made a really important point – something that I frequently speak about. And that’s the reminder that when it comes to the idea of co-design, if there is no opportunity for all stakeholders engaged to influence – ESPECIALLY in the case of diabetes, PWD – then it is not true co-design.
Too often, we see examples of services, activities and programs that don’t provide PWD that opportunity to influence. When that is the case, what we have is pure tokenism. And in my mind, tokenism is even worse than not consulting at all, because it gives the illusion of co-design without the reality of it. Too frequently I hear of organisations and services saying ‘Oh – we have these policies in place’ when truthfully, they are worth little more than the paper on which they are written because PWD do not actually have real power to effect any influence.
In my experience working in diabetes organisations, one of the things that I have come to understand as being critical is support from leadership. The role I started in 17 years ago at Diabetes Victoria could have been considered tokenism (one person ‘doing type 1 diabetes’) three days per week, without any budget only grew because then-CEO, Greg Johnson, had an attitude of ‘if we’re talking about diabetes programs services and activities there better be people with diabetes in the room talking about it with us.’ For a while, the director I reported to, Dr Ralph Audhem, a GP from Melbourne, was committed to establishing a national type 1 diabetes program that was fully staffed by people affected by people affected by diabetes.
Both were willing to grow the program through resourcing (both staff and funding), but most importantly, by listening to people with diabetes – and not just those from within the organisation – and including them in every single step of the way.
Perhaps, my most favourite example of co-design recently is the Mytonomy diabetes language matters video. Deb Greenwood in overseeing the development of the video consulted with all stakeholders, firstly to help write the script that would be used. It was honed and finetuned by repeatedly asking people to feed into what others were saying. Instead of using actors to deliver the message, Deb engaged PWD, healthcare professionals and researchers. The result is something that not only hits the mark when it comes to its messaging, but it feels wonderfully authentic and real. No wonder people have been sharing it far and wide.
I was thrilled to be able to show it as part of the introduction to the co-design symposium at ADC, and then Jane Speight shared it again the following day during her ADEA Plenary talk. (I would really encourage ANYONE involved in putting together a diabetes conference or event to find a way to fit this three minute video into the agenda! It resonates with all involved in diabetes.)
The other speakers in the symposium all shared their own examples of where the principles of co-design had been applied with great success. Melinda Seed spoke about the Type 1 Network and how that grew from a gap of providing support and information for young adults with diabetes; Frank Sita shared his experiences of being on the Perth Diabetes Care Young Adults with Diabetes Committee and Melinda Morrison provided an overview of stakeholder involvement and engagement in the NDSS Diabetes and Pregnancy priority area.

These real-life examples provided attendees with an understanding of how they too could incorporate the idea and principles of co-design in their own work – which is exactly what we hoped to achieve when designing (co-designing!!!) the session. And it seems that just maybe, we got through to some people. I’ll finish this post with this tweet from credentialled diabetes educator and midwife, Belinda Moore:
I was very lucky to be invited to attend the Roche #DiabetesMeetup held at ATTD in Vienna. About 60 advocates were brought together on the thirty-fifth floor of a building high above Vienna. I reconnected with friends and fellow advocates from Italy, Sweden, Germany, Belgium and welcomed UK advocates for the first time to the blogger group. The dynamic in this room is electrifying – these are smart, passionate, funny, outspoken, opinionated people with high expectations when it comes to their diabetes management experience – exactly the sort of people you want around you when you are developing diabetes technology solutions.

Elena from Italy.
I remain fascinated – and impressed – by these Roche events, even though this is the fourth one I’ve attended. I have a level of frustration at times when attending similar events because instead of them being used as an opportunity for engagement and interaction, they become sales pitches, with attendees being spoken at. I have sat in other events feeling as though I am being told what and how I should feel about my own diabetes with those speaking at me making all sorts of assumptions based on some ridiculous market research that involved anyone other than real people with real diabetes!
By and large, these #DiabetesMeetup events are the very opposite of that.
As I have said before, I am not naïve. I am fully aware that we as bloggers and patient advocates are worth a lot to industry. We blog, we Instagram, we Tweet, we Facebook. We have a voice and we use it. We have a platform – however big – that means we are very privileged to be able to speak about our experiences and have people listen.
By engaging with us in this way, we have become part of Roche’s – a very big drug and device company – 21st century marketing and communications plan. We are part of their PR machine. And I am absolutely okay with that. I can leave at any time. I can not write about what goes on at these events if I don’t want to.
I have also said before that it would be worse for us to not be part of their plan – or if they were stuck in the 20th century and refusing to actually work with people with diabetes.

Ute Volkmann from Roche Global doing a stellar job running the day.
The reason these events continue to leave an impression is because they are absolutely not an opportunity for Roche to lecture us and do a big whizz bang display of their technologies. Of course we see what they’re up to. But then we tell them what we think. (At the first Roche #DiabetesMeetup I attended in Munich, we were shown their in-development CGM device. The feedback wasn’t all that favourable. I have not seen or heard anything more about this product, and can only imagine that their R&D team had a lot to think about after rather negative reviews from the people who were hoped to be using the device.)
Previously, I have refused to attend advocate sessions in the past because there was an expectation that all attendees would be using the company’s product, and if not, we were expected to hide away any competing devices . Not once at these events has anyone asked me what I use, tried to give me a Roche product or suggested I use one of their devices. (For the record and full transparency, the only Roche product I use is my lancing device which I paid for myself and the lancets that come with it. I’ve not needed to buy more lancets because I think the lancet device came with about 10 of them, so I’m good until about the middle of the century.)
The big ticket item in Roche’s diabetes tech bag at present is the Eversense XL. The announcement at #DibetesMeetup that the implantable sensor now has a lifespan of 180 days. To illustrate the point, we heard that if you inserted a sensor while there was snow on the ground, you would need to replace it in the height of Summer.

Annie and I can always be trusted to bring down the overall tone of an event.
I am all for continued innovation in sensor development, and I can certainly see the appeal of the Eversense. I spoke with a couple of people at the event who were wearing them and their experience had been super positive. I’ve not worn the device and am most interested in the real life experience: how does it feel on?; how annoying is the transmitter and does it fall off?; the tape required for the transmitter to adhere to the skin – does it irritate? I am also keen to see how Eversense will be able to integrate with existing diabetes tech. And, I’m ever mindful of expected cost to the person with diabetes because I want to know if this is something that will be available and accessible to many people, or just a lucky few.
Roche followed up the blogger event with a symposium on the Friday of ATTD. It was here they announced they would be supporting JDRF’s Open Protocol proposal (which I discussed in yesterday’s post.)
While the formalities are all interesting, it is often the discussions that happen outside the official program that have real impact. I had a couple of very robust conversations about the role PWD have when working with industry. We know there are people in the diabetes community who have a complete and utter aversion to any interaction with device and drug companies.
My position on this is and has always been clear: our role is to be part of every single discussion about diabetes and every level and every step of the way. My only insistence is that there is transparency. I always disclose when I have been funded to attend an event, if I have been given product or working with any company on a project.
I was also involved in a brilliant conversation about the whole idea of sharing CGM data with loved ones. Some people were completely against the idea, unable to consider a single time when they would ever want anyone else to see their CGM numbers or find it useful. Others are big fans of share capabilities, because it makes their families feel safe when they are away. I see both sides to this story.
I had lots of chances to hear what people had been up to and how their advocacy efforts were playing out. One of the wonderful things about coming together every six months or so is that there has been time for projects to grow, blossom and show results. It is always great to hear people doing so well in their endeavours to provide support to others with diabetes.
In a connected world where I see most of these European diabetes advocates online at least every week, it is undeniable that these face-to-face opportunities provide an extra level of support and engagement. I am extraordinarily grateful to have that opportunity – to see, learn from and work with such a dynamic group of people I am fortunate to call friends.

What’s the collective noun for a group of dynamic diabetes advocates?
DISCLOSURE
Roche Diabetes Care (Global) covered my travel and accommodation costs to attend their #DiabetesMeetup Blogger event at #ATTD2018. They also assisted with providing me press registration to attend all areas of ATTD2018. As always, my agreement to attend their blogger day does not include any commitment from me, or expectation from them, to write about them, the event or their products.
Three days in Vienna is never going to be enough, and neither were three days at ATTD. But mother guilt is a very strong motivator for getting back home as quickly as possible.

This is the second ATTD conference I attended. Last year, I returned a little bewildered because it was such a different diabetes conference to what I was used to. But this year, knowing what to expect, I was ready and hit the ground running.
There will be more to come – this is the initial brain dump! But come back from more in coming weeks. Also, if you emailed me, shot me a text, Facebooked me, Tweeted me or sent me a owl last week, I’ll get back to you soon. I promise. Long days, and long nights made me a little inaccessible last week, but the 3am wake up thanks to jet lag is certainly helping me catch up!
So, some standouts for me:
DIY
The conversation shift in 12 months around DIY systems was significant. While last year it was mentioned occasionally, 2018 could have been called the ATTD of DIY APS! Which means that clearly, HCPs cannot afford to think about DIY systems as simply a fringe idea being considered by only a few.
And if anyone thinks the whole DIY thing is a passing phase and will soon go away, the announcement from Roche that they would support JDRF’s call for open protocols should set in stone that it’s not. DANA has already made this call. And smaller pump developers such as Ypsomed are making noises about doing the same. So surely, this begs to the question: Medtronic, as market leaders, where are you in this?
It was fantastic to see true patient-led innovation so firmly planted on the program over and over and over again at ATTD. After my talk at ADATS last year – and the way it was received – it’s clear that it’s time for Australian HCPs to step up and start to speak about this sensibly instead of with fear.
Nasal glucagon
Possibly one of the most brilliant things I attended was a talk about nasal glucagon, and if diabetes was a game, this would be a game changer! Alas, diabetes is not a game, but nasal glucagon is going to be huge. And long overdue.
Some things to consider here: Current glucagon ‘rescue therapy’ involves 8 steps before deliver. Not only that, but there are a lot of limitations to injectable glucagon.
Nasal glucagon takes about 30 seconds to deliver and is far easier to administer and most hypos resolved within 30 minutes of administration. There have been pivotal and real world studies and both show similar results and safety. Watch this space!
Time in Range
Another significant shift in focus is the move towards time in range as a measure of glucose management rather than just A1c. Alleluia that this is being acknowledged more and more as a useful tool, and the limitations of A1c recognised. Of course, increasing CGM availability is critical if more people are going to be able to tap into this data – this was certainly conceded as an issue.
I think that it’s really important to credit the diaTribe team for continuing to push the TIR agenda. Well done, folks!
BITS AND PIECES
MedAngel again reminded us how their simple sensor product really should become a part of everyone’s kit if they take insulin. This little slide shows the invisible problem within our invisible illness
Affordability was not left out of the discussion and thank goodness because as we were sitting there hearing about the absolute latest and greatest tech advantages, we must never forget that there are still people not able to afford the basics to keep them alive. This was a real challenge for me at ATTD last year, and as technologies become better and better that gap between those able to access emerging technology and those unable to afford insulin seems to widening. We cannot allow that to happen.
Hello T-Slim! The rumours are true – Tandem is heading outside the US with official announcements at ATTD that they will be supplying to Scandinavia and Italy in coming months. There are very, very, very loud rumours about an Australian launch soon but as my source on this is unofficial, best not to add to the conjecture.
How’s this for a soundbite:
GOLD STARS GO TO….
Massive congrats to the ATTD team on their outstanding SoMe engagement throughout the conference. Not a single ‘No cameras’ sign to be seen, instead attendees were encouraged to share information in every space at the meeting.
Aaron Kowalski from JDRF gave an inspired and inspiring talk in the Access to Novel Technologies session where he focused on the significant role PWD have in increasing access to new treatments and his absolute focus on the person with diabetes had me fist pumping with glee!
Ascensia Diabetes packed away The Grumpy Pumper into their conference bag and sent him into the conference to write and share what he learnt. Great to see another group stepping into this space and providing the means for an advocate and writer to attend the meetings and report back. You can read Grumps’ stream of consciousness here.
Dr Pratik Choudhary from the UK was my favourite HCP at ATTD with this little gem of #LangaugeMatters. Nice work, Pratik!
ANY DISAPPOINTMENTS?
Well, yes. I am still disappointed that there were no PWD speaking as PWD on the program. This is a continued source of frustration for me, especially in sessions that claim to be about ‘patient empowerment’. Also, considering that there was so much talk about ‘patient-led innovation’, it may be useful to have some of those ‘patient leaders’ on the stage talking about their motivations for the whole #WeAreNotWaiting business and where we feel we’re being let down.
I will not stop saying #NothingAboutUsWithoutUs until I feel that we are well and truly part of the planning, coordination and delivery of conferences about the health condition that affects us far more personally that any HCP, industry rep or other organisation.
DISCLOSURE
Roche Diabetes Care (Global) covered my travel and accommodation costs to attend their #DiabetesMeetup Blogger event at #ATTD2018 (more to come on that). They also assisted with providing me press registration to attend all areas of ATTD2018. As always, my agreement to attend their blogger day does not include any commitment from me, or expectation from them, to write about them, the event or their products. It is, however, worth noting that they are doing a stellar job engaging with people with diabetes, and you bet I want to say thank you to them and acknowledge them for doing so in such a meaningful way.
It’s easy to remember the difficult moments we’ve experienced at the hands of healthcare professionals who have been less than kind.
And, equally, we remember those moments where kindness was shown in spades.
I know I certainly remember moments of kindness in healthcare. And those moments transformed me. I so appreciated the kindness that came from HCPs at moments when a tsunami of grief or despair or pain or a diagnosis washed over me, knocked me to the ground and left me doubtful that I would ever be able to get back up again.
I remember kind words, the silences afforded to me giving me a moment or two (or dozens) to think, the time I was given to understand what was happening and formulate a plan to manage… I remember them all because they left me stronger, more determined, better supported and far more empowered to cope.
Kindness is a highly underrated quality in healthcare. I’m not sure how it should be included in a curriculum full of critically essential information, but it needs to be taught from the very beginning of any healthcare courses, and it’s importance highlighted and stated over and over and over again.
In the last year or so, I’ve read a few books written by (as the publicity often claims) ‘healthcare professionals turned patients’. (I’ve found this to be quite an odd term, because surely everyone at one point or another has been a patient.)
A recurring theme throughout the books is how difficult the HCPs have found it being on the other side of the HCP / patient divide. They often appear astounded at the red tape and bureaucracy they came up against, the hoops they need to jump through to receive the appropriate care, and the sheer unfriendliness of the system. And they write about the extraordinary moments of kindness that often feel far too infrequent.
Sometimes, they have written about how they didn’t realise that the way they themselves behaved could be interpreted as having a lack of consideration and kindness – explaining it was simply their manner and how they made sure they got through the day as efficiently as possible in a system often built on the foundation of complete and utter inefficiency. And yet now…now they understood.
While the books I read have been beautifully written, heart breaking at times, and often end terribly, the stories in them were not surprising. They tell truths about the system – and the lack of kindness – that people with diabetes face every day in every encounter.
When Kate Grainger launched #HelloMyNameIs, she was echoing the calls of countless people before her: please treat us like people. Please tell us what you are doing here. Please know we are scared. Please tell us who you are and what your role in my care will be.
She did it beautifully, simply, eloquently and changed the landscape of healthcare communication. I am so sad that she had to be so ill for this to happen. But her legacy is one for which I am so grateful.
Kindness in healthcare makes all the difference. Some may think it is completely unnecessary and that as long as we are receiving the right diagnosis, good care and excellent treatment, there is nothing more we need. But that is not true. Kindness adds a human element. We need warm hands, warm hearts and warm words alongside the cool tech, sterile environments and scary diagnoses.
Kindness takes no more time; it takes no more effort. But it’s effects can indeed be monumental.
As explained previously, I don’t do new year’s resolutions for the simple reason that I never stick to them. I’m unable to do the whole SMART thing and make my goals actually attainable, and so after the shortest time (a day… an hour… minutes), have thrown in the towel.
However, I am not above making resolutions for others. Because that’s the sort of person I am. Caring and sharing. Or bossy. You decide.
Here are some New Year’s resolutions for HCPs working with people with diabetes to consider:
- Use language that doesn’t stigmatise – both in front of PWD and away from us.
- And while we’re talking words: use words we understand. We may know a lot about our health condition, but we don’t necessarily understand all the medical speak. If you are talking to us, check in to make sure we actually understand what you are saying to us.
- Lose the judgement. We all judge; we do it subconsciously. Try not to.
- Remember who is in charge. While as a HCP you may have a direction that you would like us to take, or our consultations to follow, that might not work for the person with diabetes. Our diabetes; Our rules. Learn the rules and stick to them. (Also, there are not really any rules, so don’t get shitty when we seem to have no idea what we’re doing.)
- Remember this: no one wants to be unhealthy. Or rather, everyone wants to be the healthiest and best they can be. Use this as an underlying principle when meeting people with diabetes.
- Sure, offer help with setting goals. We all like to work towards something. But setting the goal is actually the easy part. Help us work out the steps to get there. If someone comes to you and wants to lose weight or reduce their A1c, that’s awesome, but they are big asks. So, tiny steps, easily achievable mini-goals and rewards for getting there.
- Acknowledge and celebrate victories. You know that person with diabetes sitting opposite you? For some, just getting there and being there is a huge achievement. Recognise that. Showing up with some data – in whatever format? That’s brilliant – so say so. Sure, it may only be three BGL readings from three different meters and all at different times, but that is a start.
- Diabetes is rarely going to be the most important thing in someone’s life. Please don’t ever expect it to be.
- Include us in every discussion about us – from letters to referring doctors or others in our healthcare team and when it comes to any results of bloody checks or scans. Make sure we have copies of these and understand what they all mean.
- Please be realistic. If someone is currently not checking their glucose levels, don’t ask them to suddenly do six checks a day, analyse the data and send you pretty graphs. Small, attainable, reasonable goals. (Once, during a period of particularly brutal burnout when my meter was not seeing the light of day, my endo asked me to do two checks a week: Monday morning before breakfast and Wednesday morning before breakfast. That was it. Next time I went back to see them, I’d not missed a single one of those checks. And even managed to do a few others as well. I felt amazingly good for actually having managed to do what was suggested and eager to keep going from there.)
- Ask us if we want to be pushed a little. Are we interested in new technologies to try, different meds to consider, a more aggressive treatment plan? Don’t assume you know the answer. Present us with the options and then help us decide if it’s something we want to try.
- Equally, if we’re pushing you because we want something new or more intensive, help us get it, learn about it and support our decision to try it.
- Do not dismiss peer networks and peer support. Offer it, direct us to it, encourage us to find it.
- Be on our side. We need champions, not critics. We need people to cheer us on from the sidelines, go into bat for us when we need an advocate and take over the baton when we’ve done all we can (and shit yeah! – that’s three sports analogies in one dot point – I deserve a gold medal!)
- Understand that diabetes does not start and end with our glucose levels. There is so much going on in our head and sometimes we need to be able to get that sorted before we can even begin to think about anything else. Get to know some diabetes-friendly psychologists, social workers and counsellors, and suggest we see them.
- Please, please, please, when it is time for our appointment, do nothing but be there with us. Of course interruptions may happen, but do apologise and excuse yourself – and do everything possible to minimise them. Look at us, take notes on a piece of paper – not a computer, and listen to us.
- Again…listen to us.
- Explain to us why you feel we need to have something done. It could be as simple as asking us to step on the scales (which often is actually not simple, but fraught) or it could be asking us to have a scary-sounding and invasive procedure. Why are you suggesting this? Is this the only course of action?
- Treat us like a person, not our faulty body part. And see all of us – not just our missing islet cells. Because really, if all you are seeing is those missing islet cells, you really are not seeing anything at all.