You are currently browsing the category archive for the ‘Engagement’ category.
ISPAD has led the way when it comes to including people with lived experience of diabetes at their annual meeting. It was the first conference to work with #dedoc° to have a voices scholarship program. The society has included people with diabetes on the organising committee for some time. ISPAD has awarded the ‘Hero Award’ which recognises the work done by people in the community. And the conference scientific program involves people with diabetes speaking and chairing sessions.
And so, it was interesting to hear someone ask at last week’s meeting in Montreal whether there should be a limit to the involvement and number of people with diabetes.
I wasn’t actually in that session, but I certainly heard about it from many others. People seem to expect me to have words to say about these sorts of questions. Turns out I do – and so do other people. And there was quite a bit of discussion – both at the conference, and in an online group after I shared the question with members.
While the question may have been well intended, (I certainly don’t believe there was any malice in asking), it did make me bristle. The idea of limiting access to a diabetes conference to people with diabetes has never sat well with me. It reeks of gatekeeping. And it also sends the message that people with diabetes are ‘allowed’ at the discretion of others rather than having a right to attend.
I think that quantifying the number of any sort of participant is problematic, but I have always liked this pie chart drawn and tweeted by James Turner (@jamesturnereux, although he appears to no longer be on the cesspit site) from a Medicine X conference in 2017. I am pretty sure that I have already shared this somewhere in the #diabetogenic archives, because I think it’s great! What I like about this is that it recognises that everyone has an equal place to be there. That equilibrium does sit well with me!

I also like the comment from my friend, and researcher and fabulous diabetes advocate, Ashley Ng. We caught up today to discuss this issue, and she said ‘I don’t agree with a maximum, but I do think we need minimum representation by people with lived experience’.
But this isn’t just a matter of representation, and it’s not simple either. There is the broader issue of people with diabetes wearing more than one hat. Some may also be researchers, clinicians, involved in technology development, industry representatives and more. This certainly does point to the complexity of the ecosystem. When looking at the number of people with lived experience of diabetes, we draw the cohort from many different spaces.
But this in itself adds to the intricacies of the situation. In fact, it is something that I have spoken and written about for decades (most recently here) and my position is very clear, albeit not especially popular with everyone. I believe that people with lived experience who wear no other hat in the healthcare space must be prioritised for positions centring lived experience at conferences, in panels, on advisory groups and anywhere people with diabetes are intended to be represented. Why? Because these are usually the ONLY way for us to get a seat at the table. Those wearing other hats may find themselves able to access other pathways via their employment or professional settings.
This is why #dedoc° generally doesn’t offer scholarships to healthcare professionals and researchers. The voices program is for people with diabetes who otherwise would not be able to find a way to attend conferences and who don’t have other prospective funding opportunities. I am aware that HCPs and researchers have limited opportunities available to them, but there are funding streams and grants, and institutional supports that are simply not open to people with lived experience who do not have any professional affiliation. Of course, (and it shouldn’t need to be said, but I’ll say it anyway), I’m not minimising the experiences of those who bring both professional and personal perspectives. But there are so very few opportunities for people with diabetes who represent as community members only to find a seat at the table. Those seats should not only be reserved for us, but we should all work to protect them.
It would be remiss of me to not point out that there are indeed unique challenges for people who straddle the professional and lived-experience divide. This article (I am a co-author) was written by people with lived experience of diabetes and wearers of other hats and addresses some of the issues faced by people in this situation.
These discussions are always interesting, but they can be uncomfortable. And also frustrating. I would hope that we are far along the lived experience inclusion road to not have to justify the rights of people with diabetes to be part of conferences and other efforts. And rather than even suggesting gatekeeping, we should be looking at more ways to make access to these spaces easier, and focused on diversity of voices. Chelcie Rice says we should bring our own chair if there isn’t one already for us. I say, bring two or three and the people to fill them too. But honestly, we should be beyond that now, right? We should simply be able to walk into any space and take a seat.
Disclosure
ISPAD invited me to speak at this year’s meeting and covered by accommodation costs. Travel was part of my role at Breakthrough T1D.
This is a transcript of a talk I gave earlier this year to a European-based health consultancy and creative agency about my take on global diabetes community-based advocacy – the opportunities and challenges. The title I was given was ‘Making Engagement the norm rather than the exception’. AI did a remarkably decent job with this transcript, but I expect that there might be some clunky language in there that I missed when I read through it on a plane after being in transit for 27 hours straight. Or, I could simply have used clunky language. Either way, it’s my fault.
I often say that community is everything, but I want to begin by saying that it’s important to understand that there is no single, homogenous diabetes community. Everyone’s diabetes experiences are different. I truly believe that there are some issues that unite us all, but really, we are a very disparate group – something I have come to understand more and more the longer I have been involved in diabetes community advocacy. This poses possibly the largest challenge for everyone in this room wanting to work with “THE diabetes community” because if you’re looking for a group that agrees on everything and believes the same thing, I’m sorry to say that you’re going to be in for quite a ride!
But it is also the biggest opportunity – and the way to get an edge – because it gives anyone who works in the diabetes space – from healthcare professionals, researchers, industry, diabetes organisations, policy makers, the media – to roll up their sleeves and make a concerted effort to talk with a wide range of people with diabetes to understand our experiences and what we need. Look, I know that it would be easier for all of you if I said, ‘Speak with one person and then you’re good to go’, but that would be a lie. Sadly, a lot of people and organisations still believe this to be the case, and I have a great example to show you why that doesn’t work.
And that example? It’s me, hi, I’m the problem, it’s me.
A number of years ago, a researcher reached out to me with an invitation to be the ‘consumer representative’ on their project. After bristling at the term “consumer”, I asked what the project was about, and this is what they said, word for word because I wrote it down and have told this story a million times as a cautionary tale: ‘It’s a project on erectile dysfunction in men with type 2 diabetes, diagnosed over the age of 65.’
There was not a note of irony in this invitation. When I pointed out that I fit literally none of the categories in the study and then went on to point out that I am a woman; I have T1D; no erectile dysfunction; diagnosed at 24; was not within a decade of 65 years of age, the response was ‘Oh, but you have diabetes, so you’ll be great’.
Friends, I would not have been great.
For the purposes of this discussion, when I say diabetes community, I am referring to people with lived experience of diabetes. There is a lot of cross over in the diabetes advocacy space, and there are many examples I can point to that show how valuable advocacy efforts can be when people with diabetes are involved in efforts led by diabetes organisations or other stakeholders. In fact, at the end of last year, we saw a brilliant example of that with Breakthrough T1D in Australia receiving $50.1 million in funding from the Australian government for their Clinical Research Network. This is the power of an organisation meaningfully engaging with their community to tell the story of why their advocacy is important. I mean, what is more compelling than hearing from people with diabetes and their families about how research holds the key to a better diabetes future?
I’d encourage you to look at Breakthrough T1D Australia’s socials to see just how beautifully they centred people with lived experience to get their message across, and how it was people with diabetes who literally marched on parliament to tell the story. The coordination of the campaign may have come from a passionate advocacy and comms team in an organisation, but the words were all people with diabetes. (For transparency: I work for Breakthrough T1D, formerly JDRF, but not for the Australian affiliate. I am, however, extraordinarily proud of what Breakthrough T1D Australia has achieved and so, so impressed with the way their communications campaigns are never about the organisation or staff, but rather about the community.)
I believe that our community excels in telling the stories of our lives with diabetes, what we need to make our lives better, what works in our communities and how we can better work together. Some standout examples of this include the #dedoc° community, and, in particular, the #dedoc° voices scholarship program. This is the only truly global community where diabetes advocates are not only present but are leading conversations. #dedoc° has no agenda other than to provide a platform for people with diabetes which results in diverse stories and experiences being heard. And it also means that organisations want to work with #dedoc° because it’s an easy way to connect with community. (And another point of transparency: I’m the Head of Advocacy for #dedoc°.)
Organisations that thrive on working with community demonstrate their commitment to improving the lives of people with diabetes in ways that matter. If you don’t know about the Sonia Nabeta Foundation (SNF), you really should! The foundation has a network of ‘warrior coordinators’ who provide peer support and a whole lot more! I have now had the honour of chairing sessions at international conferences with four of these warrior coordinators and I can say without a doubt that Hamida, Moses, Nathan and Ramadhan’s stories resonated and stayed with the audience way beyond the allotted ten minutes of their talks. Addressing the challenge of a limited workforce and resources by engaging and employing people with diabetes to educate and support younger people with diabetes is so sensible and clever. And the results are remarkable.
I have seen similar examples in India. Visiting Dr Archana Sarda’s Udaan centre in Aurangabad and Dr Krishnan Swaminathan’s centre in Coimbatore completely changed my understanding of peer-led education. And groups like the Diabesties Foundation and Blue Circle Diabetes Foundation (also in India) are prime examples of the successes we can expect when people with diabetes take charge of programs and lead diabetes education.
Seeing these examples firsthand lit a fire under me to challenge what we have been told in high-resourced countries like Australia, and here across high-income countries in Europe. Why is it that we, as people with diabetes, are told to stay in our lane and not provide education? We may be considered ‘higher resourced’, but people fall through cracks because they are not getting what they need. Health systems remain challenged and overwhelmed.
The challenge we have in places like Australia is that PWD are very clearly told that we are not qualified to provide education. Rubbish! Our lived experience expertise puts us in the prime position to do more than just tell our own story, and I believe we need to boldly push back on beliefs that only health professionals are equipped to fill education and knowledge gaps. Because in addition to what we know, the expertise we hold and our ability to speak in the language that PWD understand, we also know about ‘going to the people’ and not expecting a one size fits all approach to work.
It would be naïve to think that community-led, and -driven programs and initiatives aren’t already happening. Community is integral in providing information that PWD are desperate for, even with caveats about consulting HCPs. There are 24/7 support lines available in the community, something that is simply not available in most healthcare settings. And anyway, who better than others with diabetes to give practical advice on real life with diabetes than those walking similar paths? In the moment and with direct experience.
The #WeAreNotWaiting community was established to not just offer advice but develop technologies to improve lives of people with diabetes and continues to do so today. A five minute lurk in any of the online community groups dedicated to open-source technologies is all it takes to see people with diabetes who had been at the end of their tether with conventional care now thriving thanks to community intervention.
And that is replicated in low carb groups where community provides advice and education on how to eat in a way that is often not recommended by HCPs. People share experiences how they are flourishing thanks to making informed decisions to eat this way, and air their frustrations about how they are often derided by HCPs about those decisions. The support that comes from these groups is often just as focussed on how to deal with the healthcare environment when going against the grain (unintended pun) as sharing ideas and advice on how the science behind how low carb diets work.
T1D groups talk about incorporating adjunct therapies into their diabetes management, moving from a glucose-centric approaches to looking at other meds and interventions that can support better outcomes. GLP1s may not be approved for use by people with T1D, but they are increasingly being used off label because of their CVD and kidney protective nature. These community discussions include suggestions on how to have conversations with HCPs to ask about how adjunct therapies might help, including pushing back if there is a blanket ‘no, it’s off label’ response. Before anyone thinks this isn’t a good thing, I remind you that we still need prescriptions from our HCP before we can start on any new drug. We should be listened to when we ask to have a discussion about new and different ways to manage our diabetes.
And there are also businesses led by community that have stepped into spaces that are traditionally organisation or HCP-led. A few years ago, Aussie woman Ashley Hanger started Stripped Supply to fill a massive gap when diabetes supplies could no longer be ordered online and shipped, instead necessitating a backstep where PWD had to go into pharmacies to pick up supplies. Ashley’s start up gave the people what we wanted and meant that, for a small subscription fee, supplies could be straight to our doors again. And it’s run by community – what’s better than that?
There is contention about people with diabetes working with industry, and that is a conversation for another time. But I will say that when we have people with diabetes involved in the development of the devices that we use and/or wear on our bodies every day, the end products are better. That’s just a fact. When you have people with diabetes employed by device manufacturers writing education and instruction manuals for those devices, they make sense because they are written from the perspective of someone who actually understands the practical application of using those devices. It’s a massive opportunity for industry to engage – and employ – people with diabetes. Way to get an edge!
What I would say to everyone here today is that if you are not directly working with people with lived experience of diabetes, you are missing out on the biggest piece of the diabetes stakeholder puzzle. But you have to do it meaningfully and perhaps the biggest challenge I face is dealing with the rampant tokenism that exists in the diabetes ecosystem. For my entire advocacy career I have been urging the implementation of meaningful engagement, and to be honest, a lot of the time I feel that I have failed in those attempts. Every time I see a crappy program or campaign come out of somewhere that claims to work with community, I realise that people with diabetes are being used in possibly the most nefarious way possible: to ‘lived experience wash’ the work of the organisation. I wrote a piece earlier this year about this and was completely and utterly unsurprised to receive comments justifying poor attempts of consultation.
But then, I see something like the video I am going to finish with from Breakthrough T1D in the UK, and I know that there is intent there to do the right thing and do it properly. To involve people with diabetes from the beginning, and centre them throughout the work. The result is a beautiful piece of storytelling that has been shared across the globe. I don’t know the metrics, and quite frankly, I don’t care. All I need to see is the response from the community to know and understand that this hits the spot. And you can too with your work if you engage properly. We’re here to help.
You can watch What a Cure Feels Like, the Breakthrough T1D UK video that concluded my talk here.
Disclosure
I was invited by a health consultancy firm to give a talk to fifty people working on public-facing health campaigns (NDA, can’t say anything more) and then run a workshop about working with lived experience representatives. I was paid for my time to present and prepare for the session, and reimbursed for ground transfers to and from the location of the meeting.
Last week I was in Geneva for the 78th World Health Assembly (WHA78). It’s always interesting being at a health event that is not diabetes specific. It means that I get to learn from others working in the broader health space and see how common themes play out in different health conditions.
It’s also useful to see where there are synergies and opportunities to learn from the experiences of other health communities, and my particular focus is always on issues such as language and communications, lived experience and community-led advocacy.
What I was reminded of last week is that is that stigma is not siloed. It permeates across health conditions and is often fuelled by the same problematic assumptions and biases that I am very familiar with in the diabetes landscape.
I eagerly attended a breakfast session titled ‘Better adherence, better control, better health’ presented by the World Heart Federation and sponsored by Servier. I say eagerly, because I was keen to understand just how and why the term ‘adherence’ continues to be the dominant framing when talking about treatment uptake (and medication taking). And I wanted to understand just how this language was acceptable that this was being used so determinately in one health space when it is so unaccepted in others. This was a follow on from the event at the IDF Congress last month and built on the World Heart Foundation’s World Adherence Day.

While the diabetes #LanguageMatters movement is well established, it is by no means the only one pushing back on unhelpful terminology. There has been research into communication and language for a number of health conditions and published guidance statements for other conditions such as HIV, obesity, mental health, and reproductive health, all challenging language that places blame on individuals instead of acknowledging broader systemic barriers.
I want to say from the outset that I believe that the speakers on the panel genuinely care about improving outcomes for people. But words matter as does the meaning behind those words. And when those words are delivered through paternalistic language it sends very contradictory messages. The focus of the event was very much heart conditions, although there was a representative from the IDF on the panel (more about that later). But regardless the health condition, the messaging was stigmatising.
The barriers to people following treatment plans and taking medications as prescribed were clearly outlined by the speakers – and they are not insignificant. In fact, each speaker took time to highlight these barriers and emphasise how substantial they are. I’m wary to share any of the slides because honestly, the language is so problematic, but I am going to share this one because it shows that the speakers were very aware and transparent about the myriad reasons that someone may not be able to start, continue with or consistently follow a treatment plan.
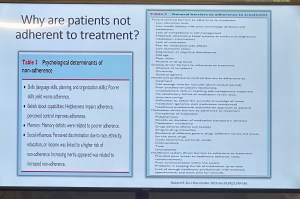
You’ll see that all the usual suspects are there: unaffordable pricing, patchy supply chains, unpleasant side effects, lack of culturally relevant options, varying levels of health literacy and limited engagement from healthcare professionals because working under conditions don’t allow the time they need.
And yet, despite the acknowledgement there is still an air of finger pointing and blaming that accompanies the messaging. This makes absolutely no sense to me. How is it possible to consider personal responsibility as a key reason for lack of engagement with treatment when the reasons are often way beyond the control of the individual?
The question should not be: Why are people not taking their medications? Especially as in so many situations medications are too expensive, not available, too complicated to manage, require unreasonable or inflexible time to take the meds, or come with side effects that significant impact quality of life. Being told to ‘push through’ those side effects without support or alternatives isn’t a solution. It is dismissive and is not in any way person-centred care.
The questions that should be asked are: How do we make meds more affordable, easier to take, and accessible? What are the opportunities to co-design treatment and medication plans with the people who are going to be following them? How do we remove the systemic barriers that make following these plans out of reach?
One of the slides presented showed the percentage people with different chronic conditions not following treatment. Have a look:

My initial thought was not ‘Look at those naughty people not doing what they’re told’. It was this: if 90% of people with a specific condition are not following the prescribed treatment plan, I would suggest – in fact, I did suggest when I took the microphone – the problem is not with the people.
It is with the treatment. Of course it is with the treatment.
The problem with the language of adherence is that it frames outcomes through the lens of personal responsibility. It absolves policy makers of any duty to act and address the structural, economic and systemic barriers that prevent people from accessing and maintaining treatment. Why would they intervene and develop policy if the issue is seen as people being lazy or not committing to their health?
And it means the healthcare professionals are let off the hook. It assumes they are the holders of all knowledge, the giver of treatment and medications, and the person in front of them is there do what they are told.
There is no room in that model for questions, preferences, or complexity. There is no room for lived experience. There are no opportunities for co-design, meaningful engagement or developing plans that are likely to result in better outcomes.
When the room was opened up to questions, I raised these concerns, and the response from the emcee was somewhat dismissive. In fact, she tried to shut me down before I had a chance to make my (short) comment and ask a question. I’ve been in this game long enough to know when to push through, so I did. I also don’t take kindly to anyone shutting down someone with lived experience, especially in a session where our perspective was seriously lacking. Her response was to suggest that diabetes is different. I suggest (actually, I know) she is wrong.
And I will also add: while there was a person with lived experience on the panel, they were given two questions and had minimal space to contribute beyond that. I understand that there were delays that meant they arrived just in time for their session, but they were not included in the list of speakers on the flyer for the event while all the health professionals and those with organisation affiliation were. There comments were at the very end of the session, and I was reminded of this piece I wrote back in 2016 where health blogger and activist Britt Johnson was expected to feel grateful that the emcee, who had ignored her throughout a panel discussion, gave her the last five minutes to contribute.
Collectively this all points to a bigger issue, and we should name that for what it is: tokenism.
I didn’t point this out at the time, but here is a free tip for all health event organisers: getting someone to emcee who is a journalist or on-air reporter does not necessarily a good emcee make. Because when you have someone with a superficial understanding of the nuance and complexity involved in living with a chronic health condition, or understand the power dynamics and sensitivities required when facilitating a conversation about long-term health conditions, you wind up with a presenter who may be able to introduce speakers, but you miss out on meaningful and empathetic framing of the situation. There are people with lived experience who are excellent emcees and moderators, and bring that authenticity to the role. Use them. (Or get someone like Femi Oke who moderated the Helmsley + Access to Medicine Foundation session later in the day. She had obviously done her homework and was absolutely brilliant.)
I know that there has been a lot of attention to language in the diabetes space. But we are not alone. In fact, so much of my understanding has come from the work done by those in the HIV/AIDS community who led the way for language reform. There are also language movements in cancer care, obesity, mental health and more. And even if there are not official guidelines, it takes nothing to listen to community voices to understand how words and communication impact us.
So where to from here? In my comment to the panel, I urged the World Heart Foundation to reconsider the name of their campaign. Rather than framing their activities around adherence, I encouraged them to look for ways to support engagement and work with communities to find a balance in their communications. I asked that they continue to focus on naming the barriers that were outlined in the presentations, and shift from ‘How to we get people to follow?’ to ‘How do we work with people to understand what it is that they can and want to follow?’.
Finally, it was great to see International Diabetes Federation VP Jackie Malouf on the program on the panel. She was there to represent the IDF, but also brought loved experience as the mother of a child with diabetes. The IDF had endorsed World Adherence Day and perhaps had seen some of the public backlash about the campaign and the IDF’s support. Jackie eloquently made the point about how the use of the word was problematic and reinforced stigma and exclusion, and that there needs to be better engagement with the community before continuing with the initiative.
One of the things of which I am most proud is seeing how the language matters movement has really made people stop and think about how we communicate about diabetes. Of course, there’s still a long way to go, but it is very clear that there have been great strides made to improve the framing of diabetes.
One area where there has been a noticeable difference is at diabetes conferences. I’m not for a moment suggesting that there is never negative language used at conferences and meetings, but the clangers stand out now and are likely to be highlighted by someone (i.e. #dedoc° voices) in the audience.
Earlier this month, the 75th IDF World Congress was held in Bangkok. Sadly, there was no livestream of the Congress, but it’s a funny thing when you have a lot of friends and colleagues (i.e. #dedoc° voices) in attendance. It meant that I had my own livestream. Sadly, the majority of what I was being sent were the language clangers.
But let’s step back a week or so to before the Congress even started. I was feeling horrendous and my brain was in a foggy, virus haze, yet I still managed to be indignant and vent at the horrendously titled ‘World Adherence Day’ which was being ‘celebrated’ on 27 March. Here is my post from LinkedIn, which has been viewed close to 12,000 times:
What I didn’t say in my post was that the IDF had eagerly endorsed the day with a media release and social media posts. My LinkedIn post took all my energy for that day, and I didn’t get a chance to follow up with the IDF. Plus, I assumed their attention would have been focused very much on the upcoming Congress.
Also, I hoped that it was a one-off misstep. I mean, surely the organisation had learnt its lesson after the Congress in South Korea when I boldly challenged incoming-president Andrew Boulton for his suggestion that people with diabetes need some ‘fear arousal’ to understand how serious diabetes is. You can see the video of my response to that at the end of this post and read the article I co-authored (Boulton was another co-author) about language here.
Alas, I was wrong. Just days before the Congress started, I saw flyers for this session shared online:
I was horrified and commented on a couple of the posts I saw. I was surprised to see some responses from advocates which amounted to ‘We can deal with it when we get there.’ Here are reasons that isn’t good enough. Firstly – not everyone is there, so all they see is the promotional of an event, comfortably using stigmatising language. It suggests that this language and the meaning behind it is okay. The discussion shouldn’t be happening after the fact. In fact, the question we should be asking is: HOW did this even happen? Where were the people with lived experience on the organising committee of the Congress speaking up about this? Did they get to see it before it was publicised? And how did the IDF miss it? This is, after all, the organisation that launched a ‘Language Philosophy’ document in 2014 (which sadly seems to be unavailable online today). It’s also the organisation that has invited me to give a number of talks about the importance of using appropriate and effective communication to IDF staff, attendees of the Young Leaders Program and as an invited speaker at a number of Congresses.
A major sponsor at the IDF Congress seemed to be very excited about the word adherence. In fact, it appeared over and over in their materials at the Congress. Here is just a couple of their questionable messaging sent to me by people (i.e. #dedoc° voices) attending the Congress:
I will point out that the IDF obviously understands the impact of stigma on people with diabetes and the harm it causes. There were sessions at the Congress dedicated to diabetes-related stigma and how to address it. In fact, I had been invited to give one of those talks. But what is disappointing is that despite this, terminology that contributes to stigma is being used without question.
I wasn’t at the Congress but from what I saw there was indeed a vibrant lived experience cohort there. #dedoc° had a scholarship program, and, as usual, there was a Living with Diabetes stream. However, I will point out that the LWD stream was not chaired by a grassroots advocate as has been the case for all previous LWD streams. It was chaired by a doctor with diabetes and while I am in no way trying to delegitimise his lived experience, I am unapologetically saying that this is a backwards step by the IDF. When there is an opportunity for a person with diabetes who is not also a health professional is given to a health professional or a researcher, that’s a missed opportunity for a person with diabetes. There were seven streams at the IDF Congress. All except for one are 100% chaired by clinicians and researchers. Only the LWD stream is open to PWD. I know that when I chaired the stream, the four members of the committee were diligent about looking through the entire and identifying any sessions that could be considered problematic for people with diabetes. It appears that didn’t happen this time.
All of this points to a persistent disconnect. It is undeniable that the language matters movement is growing, but it is still not embedded across the board—even within organisations that should know better. If we are serious about addressing stigma and centring lived experience in diabetes care, then language can’t be an afterthought or a debate to have after the posters are printed and the sessions are underway. It must be part of the planning and the review process. The easiest way to connect the dots is to ensure the lived experience community is not only present, but also listened to, respected, and in positions to influence and lead. We are long past the point where being in the room or offered a solitary seat is enough – the room is ours; we are the table.
Postscript:
I have written extensively on why language – and in particular the word ‘adherence’ – is problematic. It’s old news to me and to many others as well. This piece isn’t about that. But if you want to know why it’s problematic, here’s an old post you can read.
Disclosures:
I was an invited to give a talk about diabetes-related stigma at the IDF Congress in Bangkok, but disappointingly, had to cancel my attendance due to illness. The invitation included flights and accommodation as well as Congress registration. I was also on the program for two other sessions and was due to present to the YLD Program.
Other IDF disclosures: I have been faculty for the YLD Program for the last 10 years; I chaired the LWD Stream at the 2019 Congress and was deputy chair of the 2017 Congress.
‘Why would you bet against the type 1 community?’ That was a question asked in a session at the ISPAD conference a couple years ago. It wasn’t someone with T1D drawing attention to the community. Instead, it was said by someone working in global health who had seen the remarkable efforts such as the #WeAreNotWaiting movement and grassroots, peer-led education initiatives in low-income countries. These efforts have driven change and improved lives of people with diabetes. They have been led by those with lived experience and supported by other diabetes stakeholders. But the starting point is people directly affected by diabetes identifying a problem, solving it and leading the way. In the history of diabetes – from the first home glucose meters, to building systems leveraging off existing technologies, to global advocacy movements – community powered initiatives have been a driving force for change.
And so, here we are today, coming together once again to advocate for better equity and fairness for all people with type 1 diabetes, this time in Australia, and this time advancing access to automated insulin delivery devices (AID).
Insulin pump funding is broken. AID is standard care and yet far too many people are left unable to use the tech because of how pumps are funded in Australia. Right now, unless a person with T1D has the right level of private health insurance, or meets the criteria for the Insulin Pump Program, they must find the funding for an insulin pump. That needs to change.
We know how to do this in Australia. The reason that pump consumables are on the NDSS is thanks to community advocacy efforts back in the early 2000. And more recently massive community noise helped to get CGM onto the NDSS for all Australians. Of course, these wins worked because everyone was involved in advocacy: people with lived experience of diabetes, healthcare professionals and HCP professional groups, researchers, diabetes community groups and organisations and industry. What a lot of noise we can make when we’re singing from the same song sheet!
Right now, attentions are razor focused on improving access to automated insulin delivery systems because the evidence is clear: AID reduces diabetes distress, improves quality of life, and (for those who like numbers!), help with glucose levels. And as an added bonus for the bean counters – it’s a smart, cost-effective investment for our health system.
If AID is standard care, financial barriers preventing people from accessing it need to be eliminated.
And that’s where we would love your help.
Please sign and share the petition that has been started by Dr Ben Nash and supported by a group of people with T1D (including me). Petitions are a great way to get people talking and interested in a topic. It builds momentum and helps contribute to whole of community conversations. While we know the T1D community is already on board, we’ve now seen a number of HCPs, community groups and diabetes organisations share and promote the petition and are keen to get involved with broader advocacy efforts. That’s pretty cool!
Postscipt:
Understandably, there are questions about why this work is specific to T1D technology access. That’s a fair question and I think that our very own Bionic Wookiee provided an excellent explanation of that when he said this in a social media post earlier this week:
‘AID systems were developed for T1D (where they can track all the insulin going into the system without having to cope with the body’s variable insulin generation). So right now they mainly apply to T1D…
Expanding CGM and pump access to people with other forms of diabetes than just T1D is important for the future. Having wider access to AID for the T1D population will be a beach-head for that.‘
And in a conversation I had about this with UK diabetologist Partha Kar yesterday he cautions that there needs to be a starting point because the sheer numbers of diabetes can be daunting and tend to scare policy makers. He also points out that when it comes to outcome modifying interventions, technology is THE thing in T1D, whereas in other types of diabetes there are other options. I’ll add that those other options often have stronger evidence which is why they already have funding.
The #dedoc° symposium kicked off ATTD 2024 in the most powerful way. Four community advocates from across the globe presented on a variety of topics including access to insulin during humanitarian crises, access to diabetes care and technologies in low income settings, accessibility of technology for people with diabetes also living with disabilities, and access to research findings. You can hear the brilliant talks from #dedoc voices Leon Tribe, Tinotenda Dzitiki, NurAkca and Asra Ahmed here.
During the panel discussion, there was an important discussion about how and why it is critical for people with diabetes to be included in all conversations about diabetes. Meaningful consultation is the golden ticket here, and there were some valuable comments and suggestions about how that happens. Someone asked the question about reimbursement for lived experience expertise, an often ignored issue when it comes to people with diabetes being involved in research, programs, committees and anything else that takes our time. Our unique perspective cannot be provided by anyone else, and yet there is rarely budget to cover the costs of our participation. Sadly, it’s not routine to offer payment for our time, instead we are often made to feel that we should be grateful for a seat at the table. It’s worth reminding those who don’t value us in a financial way that WE ARE THE TABLE and without us, there wouldn’t be a place setting for anyone else.
It was clear from the conversation that diabetes advocates – even those sitting on stage at International scientific conferences – find it difficult to ask for their valuable expertise and time to be reimbursed.
I jumped off stage and made a bee line for Jazz Sethi. We do this thing at conferences that I’ve started referring to as the ‘Jazz and Renz conference special’. (You can see previous efforts here and here.) Within five minutes we’d hatched a plan for our next project, and today, we’re so excited to share it. It was clear that we need some ‘Rules of Engagement’ that provided a clear and easy way for people with diabetes and those seeking to work with us to understand not only why engagement and consultation is essential, but why it’s also essential to pay for our time.
It’s not just about reimbursement though. It’s also about recognition for that work in a multitude of ways including being included as a co-author on publications, included on programs giving presentations and having our expertise acknowledged as just as important as all other diabetes stakeholders.
And so, here are some simple guidelines that can be used by people with diabetes when working with organisations, researchers, healthcare professionals, industry and anyone else who wants out expert knowledge. Use them in your discussions with anyone who invites you to be involved in diabetes work. Print them out and take them with you when you’re meeting with anyone running a project or convening an advisory group. Share them in your networks so as many people as possible can use the information to guide discussions about ensuring our value is truly acknowledged. We hope that this will make those discussions just a little easier.
And for those who wish to work with us, have a read. If you still think that our time isn’t worth your budget, or our expertise worth real recognition, then it can only be considered that you are doing the very least to include people with diabetes. That’s tokenism. We’re not here for that anymore.




Disclosure
I was an invited speaker at ATTD 2024 where I presented on the T1D Index in my capacity as Director Community Engagement and Communications in the Global Access Team at JDRF International. I also chaired a session on access to research. ATTD covered my registration costs. My travel and accommodation were covered by #dedoc° where I am Global Head of Advocacy. I chaired the #dedoc° symposium at the conference.
Ten years ago, Australian Prime Minister Tony Abbott appointed himself as the Minister for Women. Much has been written about the message this sent and what the government of the time really thought about women, despite the carefully framed rhetoric being spewed in press releases and at doorstop press conferences. But this post is not a lesson in Australian politics. It merely sets the scene for me to speak about the underhanded ways that those whose voice should be heard are silenced.
Diabetes advocacy sits in an environment that often resists the voices of those most affected by diabetes, at times in somewhat sneaky ways. A wolf in sheep’s clothing in advocacy comes in the form of anyone claiming to advocate by ‘being the voice’ of people with diabetes, which is problematic not least because we have our own voices and don’t need others to speak for us. Being adjacent to diabetes does not give anyone license to speak on our behalf. In fact, the very idea that anyone thinks that they can represent those who should be centred is offensive.
It matters, by the way. When our insights are not the ones being heard, we find ourselves in a cycle of misunderstanding and misrepresentation. Our perspective must be heard because it is inevitably comes with the reality of diabetes. When a person with diabetes is asked about why we need to invest in better diabetes care, have better access to drugs and technology or improve funding in diabetes research, we will speak of how improved care leads to better engagement with our healthcare professionals, reduced emotional load and the resulting increased time we can spend with loved ones and being productive at work. We will speak about how increased access can equal decreased burden for us and what that means in our real lives. And we will speak about how research is the gateway for us to have better understanding of our diabetes, helping us make more informed decisions, and speak to how research has changed our lives to date. We speak about hope authentically because we hold onto it with both hands.
Someone speaking ‘on our behalf’ will inevitably focus on reducing burden to the health system (which often makes us feel as if we’re to blame for overwhelmed and overrun hospitals and adds to diabetes stigma) or resort to listing diabetes-related complications, a familiar trope that sounds like a shopping list that does well to scaring us! I spent years being a spokesperson for diabetes organisations and always ensured that the reality of day-to-day diabetes was part of the discussion, not just the rehearsed talking points that tell nothing of the people behind the numbers. Even more importantly, I learnt very early on in my own advocacy when it was not my voice that should be heard and ensured I had a network I could reach into to find the right person. I estimate that about ninety percent of the time I’m asked to give comment, I point whoever is asking in the direction of someone far better positioned to share their lived experience.
This year brought with it a new role where it was essential that I step into the background. I now find myself in the incredibly fortunate position of working with unbelievably brilliant grassroots and community advocates doing truly life changing work with people with diabetes across India. I am not here to tell their stories or about their work. I wouldn’t do it justice – I have more than enough self-awareness to know that. I recognise that they are the protagonists of their narrative. They are the ones doing living the experiences, doing the ground-breaking work, and pushing for change. My responsibility is to be an ally and a supporter, doing what I can to amplify their voices rather than overshadow them. Perhaps this speaks to my own confidence in my abilities as an advocate that I don’t feel threatened by others who are raising their voices. Effective advocacy thrives on collaboration and shared leadership, and I admire those in the advocacy world who willingly take a step back. I think it’s fair to say that others also see those who do that; and also those who do not.
There are more insidious and damaging ways that our voices are silenced. Let’s go back for a moment to our former Prime Minister. I said earlier that he made himself Minister for Women. Except, he didn’t. In fact, he abolished the position and moved it into the Office of PM and Cabinet, removing the seniority and decision-making powers it had previously held. Sure, he appointed Michaela Cash as an advisor, but this was no more than an exercise in tokenism. The reality was that the PM would have final control over decisions affecting women. Abbott bristled when questioned about his decision, refusing to listen to the myriad women and women’s groups criticising the move, instead responding defensively.
I use this as an example when consulting organisations about effective engagement and how to address commentary from the community they work with and for. Receiving criticism can be uncomfortable. However, by being open to how community responds and the feedback they generously offer, it is an opportunity for improvement and collaboration, rather than a threat to be neutralised. It’s incredibly disappointing when organisations respond by attempting to discredit or question the motives and expertise of those with lived experience or suggest that negative comments are part of efforts underpinned with ulterior motives. It’s disheartening to hear implications that individuals offering critical perspectives are merely being influenced by others, disregarding their ability to form independent thoughts and opinions. This is simply another way that community voices are effectively silenced, and proves to the community that contributions from those who should be heard are not valued at all.
I speak a lot about allyship as a pivotal force in including and amplifying rather than excluding and silencing the voices of those with lived experiences. Allyship is an active commitment to placing people with diabetes at the forefront of conversations; featuring them in all levels of decision making; putting them in the rooms where things happen. True allyship involves listening to and acting upon the needs and concerns of people with diabetes, even when what is being said is difficult to hear. What it isn’t is fantastic window dressing. We see right through that.
I wrote this piece while listening to Black Oak Ensembles 2019 album, ‘Silenced Voices’. It’s stunning.
In a month where there is A LOT of great stuff happening in the diabetes world, stop for a minute and get to know D-Coded, a brilliant new resource which helps to break down diabetes research in an accessible, informative, and authentic manner. It simplifies complex research studies and contextualises information without losing any of the insights and provides people with diabetes a starting point to better understand research, and work out how to delve deeper if we want.
One of the challenges of communicating research is that it can be a lot of detail using specialised language and complex stats and data interpretation. There may be an assumed knowledge that people simply may not have. There are acronyms, jargon, abstract concepts and the details can be lengthy and overly detailed. And that’s if we can see it! Often research papers are behind a paywall, so we can’t event see it in the first place.
Diabetes research is the reason that we are all alive today and it gives us hope for the future. At any one time, the research agenda is advancing to find ways to prevent, cure and treat all types of diabetes in ways that give me so much hope. And so, it makes sense that we should have access to it in a way to keep us engaged and interested and wanting to know more.
One of the tactics I’ve employed over the years is to ask researchers to break down their research into a tweet (280 characters or fewer), or as an elevator pitch. Most find it impossible to do. There is a language to research that can be complex, confusing, and complicated – just as there is a language to lived experience that confounds others. (Don’t believe me? Throw HbA1c, #YDMV, CGM, DIYAPS etc. around and see how people outside our community follow what we’re saying!) D-Coded does that for researchers. Everyone wins here!
It comes as no surprise that this came from the team at Diabesties. Led and powered by Jazz Sethi and involving community, it’s a project that once again shows how lived experience innovation drives change, this time by levelling the knowledge playing field.
Check it out and share as widely as you can.
DISCLOSURE
I am a Lived Experience Advisor on D-Coded. I don’t receive any payment for my involvement and am honoured to have been invited to be part of this project.
All too frequently, when talking about meaningful lived experience engagement, I hear about ‘Hard to Reach Communities’. A number of years ago, I called rubbish on that, putting a stop to any discussion that used the term as a get out of jail free card to excuse lack of diversity in lived experience perspectives.
‘People with type 2 diabetes don’t want to be case studies’ or ‘Young people with diabetes don’t respond to our call outs for surveys’ or ‘People from culturally and linguistically diverse communities won’t share their stories’ or ‘Folks in rural areas don’t come to our events’. These are just some real life examples I heard when asking why there was no diversity in the stories I was seeing.
See how the blame there is all on the people with diabetes? They don’t want, don’t respond, won’t share, won’t attends. It’s them. They’re the problem. It’s them.
I stood on stage at EASD in Stockholm last year and challenged the audience to stop using the term ‘hard to reach’. Because that’s not the case at all. The truth is that in most cases, the same old, uninventive methods are always employed. And those methods only work for a very narrow segment of the community.
I recently heard someone begrudge that all applicants who responded to a recent call out for a new committee were the same: white, had type 1 diabetes, city-dwelling. ‘Of course they are,’ I said. ‘That’s the group that loves a community advisory council and responds to an expression of interest call out on socials. They are able to attend meetings when they are scheduled, are confident to speak up and are willing to share their story, because they probably have before and received positive feedback for doing so Plus, they’re expecting everyone else at the table will look and sound just like them.’
But the lack of diversity isn’t the problem of the people who didn’t respond. It’s the problem of whoever is putting out a call and expecting people to reply because that’s how it’s Always Been Done.
This was a discussion at a meeting during last week’s American Diabetes Association Scientific Sessions. The #dedoc° voices were meeting with the ADA’s Chief Scientific Officer, Dr Bob Gabbay, and Vice President in Science & Health Care, Dr Nicole Johnson. The question about how to reach a broad audience was asked. At #dedoc°, efforts have been made to attract a diverse group of people to our scholarship program, and have, to a degree there as been some success. A glance at any one of the #docday° events, or scholarship alumni will see people who had not previously been given a platform within the diabetes community. But there is always more than can be done.
The discussion in that meeting at ADA mirrored many that happened throughout the week. And it’s not surprising that US diabetes advocate Chelcie Rice came up with the perfect way to explain how to do better at engaging with the who have previously been dismissed as ‘hard to reach’. He said: ‘You can’t just put pie in the middle of the table. Deliver the pie to where they are.’ And he’s right. Those tried and true methods that work for only one narrow segment of the community have been all about putting pie in the middle of the table, knowing that there will be some people ready with a plate and a fork. But a lot of people are not already at the table, or comfortable holding out their plate. Or maybe they don’t even like that pie. But we never find out because no effort is really made.
Chelcie once said ‘If you’re not given a seat at the table, bring your own chair‘ and I’ve repeated that quote dozens, if not hundreds of times. And his words ring very true for people like me who have felt very comfortable dragging my own chair, and one for someone else and insisting that others scramble to make room for us. But that metaphorical table isn’t enough anymore. Not everyone wants to sit at a table and we need to stop expecting that. Instead, it’s time to find people where they are – the places, the settings, the environments they feel comfortable and at home. That’s how you do engagement.

‘What would the ideal campaign about diabetes complications look like?’
What a loaded question, I thought. I was in a room full of creative consultants who wanted to have a chat with me about a new campaign they had been commissioned to develop. I felt like I was being interrogated. I was on one side of a huge table in a cavernous boardroom and opposite me, sat half a dozen consultants with digital notepads, dozens of questions, and eager, smiley looks on their faces. And very little idea of what living with diabetes is truly about, or just how fraught discussions about diabetes complications can be.
I sighed. I already had an idea of what their campaign would look like. I knew because more than two decades working as a diabetes advocate means I’ve seen a lot of it before.
‘Well,’ I started circling back to their question. ‘Probably nothing like what you have on those storyboards over there’. I indicated to the easels that had been placed around the room, each holding a covered-over poster. The huge smiles hardened a little.
Honestly, I have no idea why I get invited to these consultations. I make things very hard for the people on the other side of the table (or Zoom screen, or panel, or wherever these discussions take place).
I suppose I get brought in because I am known for being pretty direct and have lots of experience. And I don’t care about being popular or pleasing people. There is rarely ambiguity in my comments, and I can get to the crux of issue very quickly. Plus, consulting means getting paid by the hour and I can sum things up in minutes rather than an afternoon of workshops, and that means they get me in and out of the door without needing to feed me. I think the industry term for it is getting more bang for their buck.
I suggested that we start with a different question. And that question is this: ‘How do you feel when it is time for a diabetes complication screening’.
One of the consultants asked why that was a better question. I explained that it was important to understand just how people feel when it comes to discussions about complications and from there, learn how people feel when it’s time to be screened for them.
‘The two go hand in hand. I mean, if you are going to highlight the scary details of diabetes complications, surely you understand that will translate into people not necessarily rushing to find out more details.’
I told them the story I’ve told hundreds of times before – the story of my diagnosis and the images I was shown to convey all the terrible things that my life had in store now. Twenty-five years later, dozens and dozens of screening checks behind me, and no significant complication diagnosis to date, and yet, the anxiety I feel when I know it’s time for me to get my kidneys screened, or my eyes checked sends me into a spiral of fret and worry that hasn’t diminished at all over time. In fact, if anything, it has increased because of the way that we are reminded that the longer we have diabetes, the more likely we are to get complications. There is no good news here!
‘But people aren’t getting checked. They know they should, and they don’t. And some don’t know they need to. Or even that there are complications,’ came the reply from the other side of the table.
Now it was me whose face hardened.
‘Let’s unpack that for a moment,’ I said. ‘You have just made a very judgemental statement about people with diabetes. I don’t do judgement in diabetes, but if you want to lay blame, where should it lie? If you’re telling me that people don’t know they need to get checked or that there are diabetes complications, whose fault is that?’
I waited.
‘Blaming people or finding fault does nothing. That’s not going to help us here. You’ve been tasked to develop something that informs people with diabetes about complications – scary, terrifying, horrible, often painful – complications. Do you really want to open that discussion by blaming people?’
Yes, I know that not everyone with diabetes knows all about complications, and there genuinely are people out there who do not fully understand why screening is important, or what screening looks like. The spectrum of diabetes lived experience means there are people with a lot of knowledge and people with very little. But regardless of where people sit on that spectrum, complications must be spoken about with sensitivity and care.
The covers came off the posters around the room, and I was right. I’d seen it all before. There were stats showing rates of complications. More stats of how much complications cost. More stats of how many people are not getting screened for complications. More stats showing how complications can be prevented if only people got screened.
‘Thanks, I hate it,’ I thought to myself silently.
I spent the next half an hour tearing to shreds everything on those storyboards. We talked about putting humanity into the campaign and remembering that people with diabetes are already dealing with a whole lot, and adding worry and mental burden is not the way to go. I reminded them that telling us again and again and again, over and over and over the awful things that will happen to us is counterproductive. It doesn’t motivate us. It doesn’t encourage us to connect with our healthcare team. And it certainly doesn’t enamour us to whoever it is behind the campaign.
I wrapped my feedback in a bow and sent a summary email to the consultants the following day, emphatically pointing out that I am only one person with diabetes and that my comments shouldn’t be taken as gospel. Rather they should speak with lots of people with diabetes to get a sense of how many people feel. I urged them again to resist using scare tactics, or meaningless statistics. I reminded them that all aspects of the campaign – even those that might not be directed at people with diabetes – will be seen by us and we will be impacted by it. I asked that they centre people with diabetes in their work about diabetes.
But mostly, I reminded that anything to do with complications has real implications for people with diabetes. What may be a jaunt in the circus of media and PR for creative agencies is our real life. And our real life is not a media stunt.
Disclosure
I operate a freelance health consultancy. I was paid for this work because my expertise, just as the expertise of everyone with lived experience, is worth its weight in gold and we should be compensated (i.e. paid!) for it.