You are currently browsing the category archive for the ‘Communication’ category.
This is a transcript of a talk I gave earlier this year to a European-based health consultancy and creative agency about my take on global diabetes community-based advocacy – the opportunities and challenges. The title I was given was ‘Making Engagement the norm rather than the exception’. AI did a remarkably decent job with this transcript, but I expect that there might be some clunky language in there that I missed when I read through it on a plane after being in transit for 27 hours straight. Or, I could simply have used clunky language. Either way, it’s my fault.
I often say that community is everything, but I want to begin by saying that it’s important to understand that there is no single, homogenous diabetes community. Everyone’s diabetes experiences are different. I truly believe that there are some issues that unite us all, but really, we are a very disparate group – something I have come to understand more and more the longer I have been involved in diabetes community advocacy. This poses possibly the largest challenge for everyone in this room wanting to work with “THE diabetes community” because if you’re looking for a group that agrees on everything and believes the same thing, I’m sorry to say that you’re going to be in for quite a ride!
But it is also the biggest opportunity – and the way to get an edge – because it gives anyone who works in the diabetes space – from healthcare professionals, researchers, industry, diabetes organisations, policy makers, the media – to roll up their sleeves and make a concerted effort to talk with a wide range of people with diabetes to understand our experiences and what we need. Look, I know that it would be easier for all of you if I said, ‘Speak with one person and then you’re good to go’, but that would be a lie. Sadly, a lot of people and organisations still believe this to be the case, and I have a great example to show you why that doesn’t work.
And that example? It’s me, hi, I’m the problem, it’s me.
A number of years ago, a researcher reached out to me with an invitation to be the ‘consumer representative’ on their project. After bristling at the term “consumer”, I asked what the project was about, and this is what they said, word for word because I wrote it down and have told this story a million times as a cautionary tale: ‘It’s a project on erectile dysfunction in men with type 2 diabetes, diagnosed over the age of 65.’
There was not a note of irony in this invitation. When I pointed out that I fit literally none of the categories in the study and then went on to point out that I am a woman; I have T1D; no erectile dysfunction; diagnosed at 24; was not within a decade of 65 years of age, the response was ‘Oh, but you have diabetes, so you’ll be great’.
Friends, I would not have been great.
For the purposes of this discussion, when I say diabetes community, I am referring to people with lived experience of diabetes. There is a lot of cross over in the diabetes advocacy space, and there are many examples I can point to that show how valuable advocacy efforts can be when people with diabetes are involved in efforts led by diabetes organisations or other stakeholders. In fact, at the end of last year, we saw a brilliant example of that with Breakthrough T1D in Australia receiving $50.1 million in funding from the Australian government for their Clinical Research Network. This is the power of an organisation meaningfully engaging with their community to tell the story of why their advocacy is important. I mean, what is more compelling than hearing from people with diabetes and their families about how research holds the key to a better diabetes future?
I’d encourage you to look at Breakthrough T1D Australia’s socials to see just how beautifully they centred people with lived experience to get their message across, and how it was people with diabetes who literally marched on parliament to tell the story. The coordination of the campaign may have come from a passionate advocacy and comms team in an organisation, but the words were all people with diabetes. (For transparency: I work for Breakthrough T1D, formerly JDRF, but not for the Australian affiliate. I am, however, extraordinarily proud of what Breakthrough T1D Australia has achieved and so, so impressed with the way their communications campaigns are never about the organisation or staff, but rather about the community.)
I believe that our community excels in telling the stories of our lives with diabetes, what we need to make our lives better, what works in our communities and how we can better work together. Some standout examples of this include the #dedoc° community, and, in particular, the #dedoc° voices scholarship program. This is the only truly global community where diabetes advocates are not only present but are leading conversations. #dedoc° has no agenda other than to provide a platform for people with diabetes which results in diverse stories and experiences being heard. And it also means that organisations want to work with #dedoc° because it’s an easy way to connect with community. (And another point of transparency: I’m the Head of Advocacy for #dedoc°.)
Organisations that thrive on working with community demonstrate their commitment to improving the lives of people with diabetes in ways that matter. If you don’t know about the Sonia Nabeta Foundation (SNF), you really should! The foundation has a network of ‘warrior coordinators’ who provide peer support and a whole lot more! I have now had the honour of chairing sessions at international conferences with four of these warrior coordinators and I can say without a doubt that Hamida, Moses, Nathan and Ramadhan’s stories resonated and stayed with the audience way beyond the allotted ten minutes of their talks. Addressing the challenge of a limited workforce and resources by engaging and employing people with diabetes to educate and support younger people with diabetes is so sensible and clever. And the results are remarkable.
I have seen similar examples in India. Visiting Dr Archana Sarda’s Udaan centre in Aurangabad and Dr Krishnan Swaminathan’s centre in Coimbatore completely changed my understanding of peer-led education. And groups like the Diabesties Foundation and Blue Circle Diabetes Foundation (also in India) are prime examples of the successes we can expect when people with diabetes take charge of programs and lead diabetes education.
Seeing these examples firsthand lit a fire under me to challenge what we have been told in high-resourced countries like Australia, and here across high-income countries in Europe. Why is it that we, as people with diabetes, are told to stay in our lane and not provide education? We may be considered ‘higher resourced’, but people fall through cracks because they are not getting what they need. Health systems remain challenged and overwhelmed.
The challenge we have in places like Australia is that PWD are very clearly told that we are not qualified to provide education. Rubbish! Our lived experience expertise puts us in the prime position to do more than just tell our own story, and I believe we need to boldly push back on beliefs that only health professionals are equipped to fill education and knowledge gaps. Because in addition to what we know, the expertise we hold and our ability to speak in the language that PWD understand, we also know about ‘going to the people’ and not expecting a one size fits all approach to work.
It would be naïve to think that community-led, and -driven programs and initiatives aren’t already happening. Community is integral in providing information that PWD are desperate for, even with caveats about consulting HCPs. There are 24/7 support lines available in the community, something that is simply not available in most healthcare settings. And anyway, who better than others with diabetes to give practical advice on real life with diabetes than those walking similar paths? In the moment and with direct experience.
The #WeAreNotWaiting community was established to not just offer advice but develop technologies to improve lives of people with diabetes and continues to do so today. A five minute lurk in any of the online community groups dedicated to open-source technologies is all it takes to see people with diabetes who had been at the end of their tether with conventional care now thriving thanks to community intervention.
And that is replicated in low carb groups where community provides advice and education on how to eat in a way that is often not recommended by HCPs. People share experiences how they are flourishing thanks to making informed decisions to eat this way, and air their frustrations about how they are often derided by HCPs about those decisions. The support that comes from these groups is often just as focussed on how to deal with the healthcare environment when going against the grain (unintended pun) as sharing ideas and advice on how the science behind how low carb diets work.
T1D groups talk about incorporating adjunct therapies into their diabetes management, moving from a glucose-centric approaches to looking at other meds and interventions that can support better outcomes. GLP1s may not be approved for use by people with T1D, but they are increasingly being used off label because of their CVD and kidney protective nature. These community discussions include suggestions on how to have conversations with HCPs to ask about how adjunct therapies might help, including pushing back if there is a blanket ‘no, it’s off label’ response. Before anyone thinks this isn’t a good thing, I remind you that we still need prescriptions from our HCP before we can start on any new drug. We should be listened to when we ask to have a discussion about new and different ways to manage our diabetes.
And there are also businesses led by community that have stepped into spaces that are traditionally organisation or HCP-led. A few years ago, Aussie woman Ashley Hanger started Stripped Supply to fill a massive gap when diabetes supplies could no longer be ordered online and shipped, instead necessitating a backstep where PWD had to go into pharmacies to pick up supplies. Ashley’s start up gave the people what we wanted and meant that, for a small subscription fee, supplies could be straight to our doors again. And it’s run by community – what’s better than that?
There is contention about people with diabetes working with industry, and that is a conversation for another time. But I will say that when we have people with diabetes involved in the development of the devices that we use and/or wear on our bodies every day, the end products are better. That’s just a fact. When you have people with diabetes employed by device manufacturers writing education and instruction manuals for those devices, they make sense because they are written from the perspective of someone who actually understands the practical application of using those devices. It’s a massive opportunity for industry to engage – and employ – people with diabetes. Way to get an edge!
What I would say to everyone here today is that if you are not directly working with people with lived experience of diabetes, you are missing out on the biggest piece of the diabetes stakeholder puzzle. But you have to do it meaningfully and perhaps the biggest challenge I face is dealing with the rampant tokenism that exists in the diabetes ecosystem. For my entire advocacy career I have been urging the implementation of meaningful engagement, and to be honest, a lot of the time I feel that I have failed in those attempts. Every time I see a crappy program or campaign come out of somewhere that claims to work with community, I realise that people with diabetes are being used in possibly the most nefarious way possible: to ‘lived experience wash’ the work of the organisation. I wrote a piece earlier this year about this and was completely and utterly unsurprised to receive comments justifying poor attempts of consultation.
But then, I see something like the video I am going to finish with from Breakthrough T1D in the UK, and I know that there is intent there to do the right thing and do it properly. To involve people with diabetes from the beginning, and centre them throughout the work. The result is a beautiful piece of storytelling that has been shared across the globe. I don’t know the metrics, and quite frankly, I don’t care. All I need to see is the response from the community to know and understand that this hits the spot. And you can too with your work if you engage properly. We’re here to help.
You can watch What a Cure Feels Like, the Breakthrough T1D UK video that concluded my talk here.
Disclosure
I was invited by a health consultancy firm to give a talk to fifty people working on public-facing health campaigns (NDA, can’t say anything more) and then run a workshop about working with lived experience representatives. I was paid for my time to present and prepare for the session, and reimbursed for ground transfers to and from the location of the meeting.
Last week I was in Geneva for the 78th World Health Assembly (WHA78). It’s always interesting being at a health event that is not diabetes specific. It means that I get to learn from others working in the broader health space and see how common themes play out in different health conditions.
It’s also useful to see where there are synergies and opportunities to learn from the experiences of other health communities, and my particular focus is always on issues such as language and communications, lived experience and community-led advocacy.
What I was reminded of last week is that is that stigma is not siloed. It permeates across health conditions and is often fuelled by the same problematic assumptions and biases that I am very familiar with in the diabetes landscape.
I eagerly attended a breakfast session titled ‘Better adherence, better control, better health’ presented by the World Heart Federation and sponsored by Servier. I say eagerly, because I was keen to understand just how and why the term ‘adherence’ continues to be the dominant framing when talking about treatment uptake (and medication taking). And I wanted to understand just how this language was acceptable that this was being used so determinately in one health space when it is so unaccepted in others. This was a follow on from the event at the IDF Congress last month and built on the World Heart Foundation’s World Adherence Day.

While the diabetes #LanguageMatters movement is well established, it is by no means the only one pushing back on unhelpful terminology. There has been research into communication and language for a number of health conditions and published guidance statements for other conditions such as HIV, obesity, mental health, and reproductive health, all challenging language that places blame on individuals instead of acknowledging broader systemic barriers.
I want to say from the outset that I believe that the speakers on the panel genuinely care about improving outcomes for people. But words matter as does the meaning behind those words. And when those words are delivered through paternalistic language it sends very contradictory messages. The focus of the event was very much heart conditions, although there was a representative from the IDF on the panel (more about that later). But regardless the health condition, the messaging was stigmatising.
The barriers to people following treatment plans and taking medications as prescribed were clearly outlined by the speakers – and they are not insignificant. In fact, each speaker took time to highlight these barriers and emphasise how substantial they are. I’m wary to share any of the slides because honestly, the language is so problematic, but I am going to share this one because it shows that the speakers were very aware and transparent about the myriad reasons that someone may not be able to start, continue with or consistently follow a treatment plan.
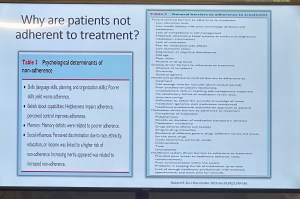
You’ll see that all the usual suspects are there: unaffordable pricing, patchy supply chains, unpleasant side effects, lack of culturally relevant options, varying levels of health literacy and limited engagement from healthcare professionals because working under conditions don’t allow the time they need.
And yet, despite the acknowledgement there is still an air of finger pointing and blaming that accompanies the messaging. This makes absolutely no sense to me. How is it possible to consider personal responsibility as a key reason for lack of engagement with treatment when the reasons are often way beyond the control of the individual?
The question should not be: Why are people not taking their medications? Especially as in so many situations medications are too expensive, not available, too complicated to manage, require unreasonable or inflexible time to take the meds, or come with side effects that significant impact quality of life. Being told to ‘push through’ those side effects without support or alternatives isn’t a solution. It is dismissive and is not in any way person-centred care.
The questions that should be asked are: How do we make meds more affordable, easier to take, and accessible? What are the opportunities to co-design treatment and medication plans with the people who are going to be following them? How do we remove the systemic barriers that make following these plans out of reach?
One of the slides presented showed the percentage people with different chronic conditions not following treatment. Have a look:

My initial thought was not ‘Look at those naughty people not doing what they’re told’. It was this: if 90% of people with a specific condition are not following the prescribed treatment plan, I would suggest – in fact, I did suggest when I took the microphone – the problem is not with the people.
It is with the treatment. Of course it is with the treatment.
The problem with the language of adherence is that it frames outcomes through the lens of personal responsibility. It absolves policy makers of any duty to act and address the structural, economic and systemic barriers that prevent people from accessing and maintaining treatment. Why would they intervene and develop policy if the issue is seen as people being lazy or not committing to their health?
And it means the healthcare professionals are let off the hook. It assumes they are the holders of all knowledge, the giver of treatment and medications, and the person in front of them is there do what they are told.
There is no room in that model for questions, preferences, or complexity. There is no room for lived experience. There are no opportunities for co-design, meaningful engagement or developing plans that are likely to result in better outcomes.
When the room was opened up to questions, I raised these concerns, and the response from the emcee was somewhat dismissive. In fact, she tried to shut me down before I had a chance to make my (short) comment and ask a question. I’ve been in this game long enough to know when to push through, so I did. I also don’t take kindly to anyone shutting down someone with lived experience, especially in a session where our perspective was seriously lacking. Her response was to suggest that diabetes is different. I suggest (actually, I know) she is wrong.
And I will also add: while there was a person with lived experience on the panel, they were given two questions and had minimal space to contribute beyond that. I understand that there were delays that meant they arrived just in time for their session, but they were not included in the list of speakers on the flyer for the event while all the health professionals and those with organisation affiliation were. There comments were at the very end of the session, and I was reminded of this piece I wrote back in 2016 where health blogger and activist Britt Johnson was expected to feel grateful that the emcee, who had ignored her throughout a panel discussion, gave her the last five minutes to contribute.
Collectively this all points to a bigger issue, and we should name that for what it is: tokenism.
I didn’t point this out at the time, but here is a free tip for all health event organisers: getting someone to emcee who is a journalist or on-air reporter does not necessarily a good emcee make. Because when you have someone with a superficial understanding of the nuance and complexity involved in living with a chronic health condition, or understand the power dynamics and sensitivities required when facilitating a conversation about long-term health conditions, you wind up with a presenter who may be able to introduce speakers, but you miss out on meaningful and empathetic framing of the situation. There are people with lived experience who are excellent emcees and moderators, and bring that authenticity to the role. Use them. (Or get someone like Femi Oke who moderated the Helmsley + Access to Medicine Foundation session later in the day. She had obviously done her homework and was absolutely brilliant.)
I know that there has been a lot of attention to language in the diabetes space. But we are not alone. In fact, so much of my understanding has come from the work done by those in the HIV/AIDS community who led the way for language reform. There are also language movements in cancer care, obesity, mental health and more. And even if there are not official guidelines, it takes nothing to listen to community voices to understand how words and communication impact us.
So where to from here? In my comment to the panel, I urged the World Heart Foundation to reconsider the name of their campaign. Rather than framing their activities around adherence, I encouraged them to look for ways to support engagement and work with communities to find a balance in their communications. I asked that they continue to focus on naming the barriers that were outlined in the presentations, and shift from ‘How to we get people to follow?’ to ‘How do we work with people to understand what it is that they can and want to follow?’.
Finally, it was great to see International Diabetes Federation VP Jackie Malouf on the program on the panel. She was there to represent the IDF, but also brought loved experience as the mother of a child with diabetes. The IDF had endorsed World Adherence Day and perhaps had seen some of the public backlash about the campaign and the IDF’s support. Jackie eloquently made the point about how the use of the word was problematic and reinforced stigma and exclusion, and that there needs to be better engagement with the community before continuing with the initiative.
It’s not an exaggeration when I say that I give thanks to Frederick Banting every single day. I have a photo of him in my office next to an artwork of the word HOPE. And anytime I am sitting at my desk working or sitting in my office reading and find myself looking at the photo, I say these words: ‘Thank you for my life’.
The story of the discovery of insulin has been told many times. There are some excellently researched and detailed accounts of what it took to get to the ‘Eureka!’ moment, as well as documentaries and a couple of feature length movies. But despite having a dozen or so books on my shelf that tell the story, I was so excited to order this version:
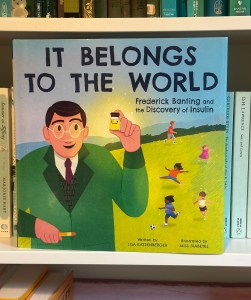
‘It Belongs to the World’ is a gorgeous children’s book by Lisa Katzenberger, and illustrated by the supremely talented Janina Gaudin, (better known online as Miss Diabetes), is a truly beautiful retelling of the story.
While it would make sense to say that this book would make a great gift for a child with diabetes, or parent living with diabetes to read to their kids, really, it’s is a book for everyone. Stories like this should be told over and over, and not just to those of us for whom it is personally relevant. Everyone should learn about the brilliance of scientific discovery. It’s a reminder of the importance of research, and how research saves lives each and every day. It serves to encourage us to get behind research efforts, as a participant or donor if possible. And it gives hope for what still lies ahead.
Oh, and it’s always good to support creators in our community. What a brilliant awareness raising effort from Janina and Lisa. Go get your copy now!
Disclosures
None! I paid for my own copy of this book through my local bookstore. They had to get it in, so you may need to order it. (Or it’s available to order through Amazon.)
One of the things of which I am most proud is seeing how the language matters movement has really made people stop and think about how we communicate about diabetes. Of course, there’s still a long way to go, but it is very clear that there have been great strides made to improve the framing of diabetes.
One area where there has been a noticeable difference is at diabetes conferences. I’m not for a moment suggesting that there is never negative language used at conferences and meetings, but the clangers stand out now and are likely to be highlighted by someone (i.e. #dedoc° voices) in the audience.
Earlier this month, the 75th IDF World Congress was held in Bangkok. Sadly, there was no livestream of the Congress, but it’s a funny thing when you have a lot of friends and colleagues (i.e. #dedoc° voices) in attendance. It meant that I had my own livestream. Sadly, the majority of what I was being sent were the language clangers.
But let’s step back a week or so to before the Congress even started. I was feeling horrendous and my brain was in a foggy, virus haze, yet I still managed to be indignant and vent at the horrendously titled ‘World Adherence Day’ which was being ‘celebrated’ on 27 March. Here is my post from LinkedIn, which has been viewed close to 12,000 times:
What I didn’t say in my post was that the IDF had eagerly endorsed the day with a media release and social media posts. My LinkedIn post took all my energy for that day, and I didn’t get a chance to follow up with the IDF. Plus, I assumed their attention would have been focused very much on the upcoming Congress.
Also, I hoped that it was a one-off misstep. I mean, surely the organisation had learnt its lesson after the Congress in South Korea when I boldly challenged incoming-president Andrew Boulton for his suggestion that people with diabetes need some ‘fear arousal’ to understand how serious diabetes is. You can see the video of my response to that at the end of this post and read the article I co-authored (Boulton was another co-author) about language here.
Alas, I was wrong. Just days before the Congress started, I saw flyers for this session shared online:
I was horrified and commented on a couple of the posts I saw. I was surprised to see some responses from advocates which amounted to ‘We can deal with it when we get there.’ Here are reasons that isn’t good enough. Firstly – not everyone is there, so all they see is the promotional of an event, comfortably using stigmatising language. It suggests that this language and the meaning behind it is okay. The discussion shouldn’t be happening after the fact. In fact, the question we should be asking is: HOW did this even happen? Where were the people with lived experience on the organising committee of the Congress speaking up about this? Did they get to see it before it was publicised? And how did the IDF miss it? This is, after all, the organisation that launched a ‘Language Philosophy’ document in 2014 (which sadly seems to be unavailable online today). It’s also the organisation that has invited me to give a number of talks about the importance of using appropriate and effective communication to IDF staff, attendees of the Young Leaders Program and as an invited speaker at a number of Congresses.
A major sponsor at the IDF Congress seemed to be very excited about the word adherence. In fact, it appeared over and over in their materials at the Congress. Here is just a couple of their questionable messaging sent to me by people (i.e. #dedoc° voices) attending the Congress:
I will point out that the IDF obviously understands the impact of stigma on people with diabetes and the harm it causes. There were sessions at the Congress dedicated to diabetes-related stigma and how to address it. In fact, I had been invited to give one of those talks. But what is disappointing is that despite this, terminology that contributes to stigma is being used without question.
I wasn’t at the Congress but from what I saw there was indeed a vibrant lived experience cohort there. #dedoc° had a scholarship program, and, as usual, there was a Living with Diabetes stream. However, I will point out that the LWD stream was not chaired by a grassroots advocate as has been the case for all previous LWD streams. It was chaired by a doctor with diabetes and while I am in no way trying to delegitimise his lived experience, I am unapologetically saying that this is a backwards step by the IDF. When there is an opportunity for a person with diabetes who is not also a health professional is given to a health professional or a researcher, that’s a missed opportunity for a person with diabetes. There were seven streams at the IDF Congress. All except for one are 100% chaired by clinicians and researchers. Only the LWD stream is open to PWD. I know that when I chaired the stream, the four members of the committee were diligent about looking through the entire and identifying any sessions that could be considered problematic for people with diabetes. It appears that didn’t happen this time.
All of this points to a persistent disconnect. It is undeniable that the language matters movement is growing, but it is still not embedded across the board—even within organisations that should know better. If we are serious about addressing stigma and centring lived experience in diabetes care, then language can’t be an afterthought or a debate to have after the posters are printed and the sessions are underway. It must be part of the planning and the review process. The easiest way to connect the dots is to ensure the lived experience community is not only present, but also listened to, respected, and in positions to influence and lead. We are long past the point where being in the room or offered a solitary seat is enough – the room is ours; we are the table.
Postscript:
I have written extensively on why language – and in particular the word ‘adherence’ – is problematic. It’s old news to me and to many others as well. This piece isn’t about that. But if you want to know why it’s problematic, here’s an old post you can read.
Disclosures:
I was an invited to give a talk about diabetes-related stigma at the IDF Congress in Bangkok, but disappointingly, had to cancel my attendance due to illness. The invitation included flights and accommodation as well as Congress registration. I was also on the program for two other sessions and was due to present to the YLD Program.
Other IDF disclosures: I have been faculty for the YLD Program for the last 10 years; I chaired the LWD Stream at the 2019 Congress and was deputy chair of the 2017 Congress.
When the clock ticked over into 2025, I had no intention of even considering coming up with New Year’s resolutions that would shape my new year. But with all that is going on in the world, I’ve given myself permission to reconsider and do all I can to stick to it. And I’m encouraging everyone I know to make the same resolution.
And that resolution is to do a health literacy check-up and to actively pushback against misinformation. There has never been a time when being health literate is more important. I thought that during the COVID years as we received a daily onslaught of misinformation about vaccines, bogus treatments (bleach, anyone?), outright lies (“it’s just a cold”) and conspiracy theories (“BigVax is behind it all”). But how naïve I was. Those days seems like just a warm-up for what is happening today.
I’m in Australia, but I don’t for one moment think we are immune to the madness sweeping the world. But if you are shaking your head and laughing a little when RFK Jr spews his anti-vax, anti-fluoride, anti-science agenda, or Dr Oz uses his latest pseudoscience claim as the foundation for whatever supplement he is selling, you’re not grasping the seriousness of what is going on. Before we Aussies get too smug, we should remember our own backyard isn’t devoid of charlatans, and it’s only a matter of time before someone like Pete Evans is taken seriously in public health discussions. Think I’m over-reacting? He already made a run for the senate. How long before a conservative party sweeps him into their fold?
I think it’s safe to say that we have moved beyond this sort of misinformation being a fringe issue amongst ‘crunchy’ parents, trad wives and ‘wellness’ influencers. And Gwyneth Paltrow.
Health misinformation is deliberate and it’s mainstream, and protecting yourself against it isn’t optional – it’s essential.
Up until now there have been guardrails in place to protect public health. Boards and regulatory agencies have existed to ensure medical safety and provide us with confidence that there are processes in place to determine the safety of drugs, devices, healthcare programs. Guidelines are based on robust and rigorous research and are developed using evidence and expert consensus. (Side bar: Have people with lived experience been involved in these practises? Absolutely not enough. Could this be better? Absolutely yes.)
Critical thinkers understand that science is not static. We understand that science changes as evidence evolves. We also understand that we don’t have to follow guidelines blindly. We should understand and consider them. And then use them to make informed health choices. I repeatedly say this to anyone who questions off label healthcare (my favourite kind of healthcare!): ‘I understand guidelines and learn the rules so I can break them safely’. That’s what being health literate does – it gives me an understanding of risks and benefits to make decisions about my health and what works best for me. And it gives me confidence to spot and push back on misinformation.
Critical thinkers also know that questioning medical advice is not the same as embracing conspiracy theories. It doesn’t mean throwing the baby out with the bathwater as you hastily reject modern medicine in favour of snake oil salespeople. It certainly doesn’t mean denying the effectiveness of a vaccines. And it doesn’t mean trusting Instagram wellness influencers.
More than ever, now is the time to do some questioning – to question who is spreading health information and consider their motives. What are they selling? (Case in point: Jessie Inchauspe who offensively calls herself ‘Glucose Goddess’ while selling her ridiculous ‘Anti Spike’ rubbish as she spreads fear about perfectly normal glucose fluctuations in people without diabetes). And a question that right now should be front of everyone’s mind: What power grab is behind the way someone is positioning themselves as an oracle of health information?
This post is about health literacy in general, but because this blog is called ‘Diabetogenic’ and I have diabetes, most people reading will be directly impacted by diabetes. And if there is any silver lining in this shitshow, it’s this: We’ve been dealing with health misinformation about our condition for decades, so in some ways, we’re probably ahead of the curve. We’ve had to wade through the myriad cures and magic therapies, the serums and pseudo-therapies. And the cinnamon – so much cinnamon! We’ve been standing up for science, challenging misinformation, and ensuring that diabetes health therapies are based on evidence, not fairytales. We’ve expected truth in our healthcare. It’s seemed the normal thing to do. Now it feels like a radical act to be a critical thinker.
We are a crucial point because health is being weaponised more than ever. Someone told me the other day that my lane is diabetes and health, and I should leave politics out of it. It’s laughable (and terrifying) to think that anyone doesn’t understand that health is political. It always has been. And even more so right now. We are seeing in real time political figures (and rich white men who own electric car companies) weaponise health misinformation for their own agendas, and scarily people are listening to them. They are elevating unqualified voices and aligning with conspiracy theorists, giving dangerous misinformation legitimacy. (And if you think that it’s all eerily familiar, you’re right. It’s already happened with climate change.)
Your radical act is to be smarter, to be more critical, to question sources and motives; follow reputable sources, don’t share viral posts before fact checking (Snopes is super useful here). Don’t reject credible advice and information in favour of conspiracy theories. Stack your bookshelves with books by qualified experts (I’d recommend starting with Jen Gunter’s holy trinity – The Vagina Bible, The Menopause Manifest and Blood and Emma Becket’s You Are More Than What You Eat), including lived experience experts who base their healthcare on legitimate evidence. Follow diabetes organisations like Breakthrough T1D (JDRF in Australia) for research updates and community efforts and be smart about which community-based groups you join. If moderators are not calling out health misinformation, I’d be questioning just how the group is contributing to diabetes wellbeing.
We know knowledge is power. But that knowledge base has to be grounded in fact, not fiction. Health literacy is critical because misinformation isn’t going anywhere, and neither are the people pushing it for profit and power. My resolution is to sharpen my critical thinking skills, ask questions, and refuse to let bad science set us backwards and cast a dark shadow over the health landscape. Who knew something so fundamental could be such a radical act?

Colour me unsurprised they couldn’t back up their claim with evidence.
I’ve been wondering how different diabetes would be if all we needed to worry about was the actual tasks of doing diabetes. ‘All’ doesn’t sound right, because I know it would certainly still be a lot. Diabetes tasks are many and constant. But if the noise disappeared and with it all the other factors that made diabetes more difficult, how much easier would it be?
If the gatekeeping disappeared and we could have access to what we need without having to jump through hoops to prove ourselves worthy, wouldn’t that make it easier?
If we had access to the best technologies and drugs when we need them, and could change as we needed, wouldn’t that make it easier?
If the judgement disappeared and we weren’t worried about how others perceived our efforts, wouldn’t that make it easier?
If the stigma vanished and we weren’t concerned about what others thought about diabetes in general, or felt that they had the right to comment on our diabetes, wouldn’t that make it easier?
If the shame and the blame wasn’t there, and we didn’t have the fingers pointing to us for getting diabetes or our diabetes outcomes, wouldn’t that make it easier?
If scare tactics were no longer deployed and we weren’t constantly being warned about all the things that could go wrong and how, if they did, it was our fault, wouldn’t that make it easier
If the fear arousal disappeared along with the numbers warning us that diabetes increased our chances of getting everything bad in the world or that we were burdening the health system, wouldn’t that make it easier?
If the not believing disappeared and we were listening to and believed and respected, so we didn’t feel that we were begging for what is even just basic care, wouldn’t that make it easier?
If the minimising of how we felt and what we were experiencing stopped, wouldn’t that make it easier?
If the grading A1Cs disappeared, so we weren’t being told that we were failing diabetes, or acing it, or oscillating between the two, wouldn’t that make it easier?
If mental health care was diabetes care and diabetes care always included mental health care, wouldn’t that make it easier?
If the idea that someone needed to speak for us and ‘be our voice’ was replaced with people with diabetes being platformed and amplified instead of silenced, wouldn’t that make it easier?
If peer support was routinely encouraged and peer-led education was normalised, wouldn’t that make it easier?
If the language around diabetes fostered attitudes of care and support, rather than bias and battles, wouldn’t that make it easier?
If claims of community engagement were real instead of nothing more than window dressing, wouldn’t that make it easier?
If we traded in hope rather than doom, and didn’t position diabetes as a battle or never-ending exhausting fight, wouldn’t that make it easier?
Because as it stands, diabetes is hard enough, but all the other things make it even harder. But the good news is that these things are often simple enough to address, simple enough to remedy, simple enough to change.
I do wish that these were the things that were front of mind when strategies developed, campaigns designed, and policies changed. That’s actually an easy part. When people with diabetes drive the diabetes agenda, everything is better. And easier for us.
So, ask yourself, are you standing in the way of making it easier for us?

So often, there is amazing work being done in the diabetes world that is driven by or involves people with lived experience. Often, this is done in a volunteer capacity – although when we are working with organisations, I hope (and expect) that community members are remunerated for their time and expertise. Of course, there are a lot of organisations also doing some great work – especially those that link closely with people with diabetes through deliberate and meaningful community engagement.
Here are just a few things that involve community members that you can get involved in!
AID access – the time is now!
It’s National Diabetes Week in Australia and if you’ve been following along, you’ll have seen that technology access is very much on the agenda. I’m thrilled that the work I’ve been involved in around AID access (in particular fixing access to insulin pumps in Australia) has gained momentum and put the issue very firmly on the national advocacy agenda, which was one of the aims of the group when we first started working together. Now, we have a Consensus Statement endorsed by community members and all major Australian diabetes organisations, a key recommendation in the recently released Parliamentary Diabetes Inquiry and widening awareness of the issue. But we’re not done – there’s still more to do. Last week I wrote about how now we need the community to continue their involvement and make some noise about the issue. This update provides details of what to do next.
And to quickly show your support, sign the petition here.
Language Matters pregnancy
Earlier this week we saw the launch of a new online survey about the experiences of people with diabetes before, during and after pregnancy, specifically the language and communication used around and to them. Language ALWAYS matters and it doesn’t take much effort to learn from people with diabetes just how much it matters during the especially vulnerable time when pregnancy is on the discussion agenda. And so, this work has been very much powered by community, bringing together lots of people to establish just how people with diabetes can be better supported during this time.
Congratulations to Niki Breslin-Brooker for driving this initiative, and to the team of mainly community members along with HCPs. This has all been done by volunteers, out of hours, in between caring for family, managing work and dealing with diabetes. It’s an honour to work with you all, and a delight to share details of what we’ve been up to!
Have a look at some of the artwork that has been developed to accompany the work. What we know is that it isn’t difficult to make a change that makes a big difference. The phrases you’ll see in the artworks that are being rolled out will be familiar to many people with diabetes. I know I certainly heard most of them back when I was planning for pregnancy – two decades ago. As it turns out, people are still hearing them today. We can, and need to change that!
You can be a part of this important work by filling in this survey which asks for your experiences. It’s for people with diabetes and partners, family members and support people. They survey will be open until the end of September and will inform the next stage of this work – a position statement about language and communication to support people with diabetes.
How do I get involved in research?
One of the things I am frequently asked by PWD is how to learn about and get involved in research studies. Some ideas for Aussies with diabetes: JDRF Australia remains a driving force in type 1 diabetes research across the country, and a quick glance at their website provides a great overview. All trials are neatly located on one page to make it easy to see what’s on the go at the moment and to see if there is anything you can enrol in.
Another great central place to learn about current studies is the Diabetes Technology Research Group website.
ATIC is the Australasian Type 1 Diabetes Immunotherapy Collaboration and is a clinical trials network of adult and paediatric endocrinologists, immunologists, clinical trialists, and members of the T1Dcommunity across Australia and New Zealand, working together to accelerate the development and delivery of immunotherapy treatments for people with type 1 diabetes. More details of current research studies at the centre here.
HypoPAST
HypoPAST stands for Hypoglycaemia Prevention, Awareness of Symptoms and Treatment, and is an innovative online program designed to assist adults with type 1 diabetes in managing their fear of hypoglycaemia. The program focuses on hypoglycaemia prevention, awareness of symptoms, and treatment, offering a comprehensive range of resources, including information, activities, and videos. Study participants access HypoPAST on their computers, tablets, or smartphones.
This study is essential as it harnesses technology to provide practical tools for better diabetes management, addressing a critical need in the diabetes community. By reducing the anxiety associated with hypoglycaemia and improving symptom awareness and treatment strategies, HypoPAST has the potential to enhance the quality of life for individuals with type 1 diabetes.
The study is being conducted by the ACBRD and is currently recruiting participants. It’s almost been fully recruited for, but there are still places. More information here about how to get involved.
Type 1 Screen
Screening for T1D has been very much a focus of scientific conferences this year. At the recent American Diabetes Association Scientific Sessions, screening and information about the stages of T1D were covered in a number of sessions and symposia. Here in Australia. For more details about what’s being done in Australia in this space, check out Type 1 Screen.
And something to read
This article was published in The Lancet earlier in the year, but just sharing here for the first time. The article is about the importance of genuine consumer and community involvement in diabetes care, emphasising the benefits and challenges of ensuring diverse and representative participation to meet the community’s needs effectively.
I spend a lot of time thinking a lot about genuine community involvement in diabetes care and how people with diabetes can contribute to that ‘from the inside’. And by ‘inside’ I mean diabetes organisations, industry, healthcare settings and in research. I may be biased, but I think we add something. I’m grateful that others think that too. But not always. Sometimes, our impact is dismissed or minimised, as are the challenges we face when we act in these roles. I don’t speak for anyone else, but in my own personal instance, I start and end as a person with diabetes. I may work for diabetes organisations, have my own health consultancy, and spend a lot of time volunteering in the diabetes world, but what matters at the end of the day and what never leaves me is that I am a person living with diabetes. And I would expect that is how others would regard me too, or at least would remember that. It’s been somewhat shocking this year to see that some people seem to forget that.
Final thoughts…
Recently when I was in New York at Breakthrough T1D headquarters, I realised just how many people there are in the organisation living with the condition. It’s somewhat confronting – in a good way! – to realise that there are so many people with lived experience working with – very much with – the community. And it’s absolutely delightful to be surrounded by people with diabetes at all levels of the organisation – including the CEO. But you don’t have to have diabetes to work in diabetes. Some of the most impactful people I’ve worked with didn’t live with the condition. But being around people with diabetes as much as possible was important to them. It’s really easy to do when people with diabetes are on staff! I first visited the organisation’s office years ago – long before working with them – to give a talk about language and diabetes. One of the things that stood out for me back then was just how integral lived experience was at that organisation. From the hypo station (clearly put together by PWD who knew they would probably need to use the supplies!) to the conversations with the team, community was in the DNA of the place. As staff, I’ve now visited HQs a few times, and I’ve felt that even more keenly. Walking through the office a couple of weeks ago, I saw this on the desk of one of my colleagues and I couldn’t stop laughing when I saw it. IYKYK – and we completely knew!

DISCLOSURES (So many!)
I was part of the group working on the AID Consensus Statement, and the National AID Access Summit that led to the statement.
I am on the team working on the Language Matters Diabetes and Pregnancy initiative.
I was a co-author on the article, Living between two worlds: lessons for community involvement.
I am an investigator on the HypoPAST study.
My contribution to all these initiatives has been voluntary
I am a representative on the ATIC community group, for which I receive a gift voucher honorarium after attending meetings.
I work for Breakthrough T1D (formerly JDRF).
It’s never hard to find a source of diabetes stigma. Because sadly, it’s all around us. And right now, the source seems to be much of the discussion about the report from the Australian Parliamentary Inquiry into Diabetes.
Yes, I was very excited about the report last week when I was writing about the recommendations and accompanying content about increasing access to pumps and AID systems. That was incredible news, and it was terrific to see that the community-led efforts were met with such a positive outcome.
But the messaging more broadly hasn’t been so great and it’s very disappointing.
Disappointing, but not surprising really. After all, the inquiry was for diabetes and obesity. Last week, I said that people with T2D deserve the same attention as people with T1D when it comes to advocacy efforts and campaigns. Well, so do people living with obesity. When the inquiry was first announced, I remember reading through its terms of reference and feeling my heart sink. These are two separate and equally important health issues that need focused attention. And within that, diabetes itself comprises different types; again, all equally important and requiring specific attention.
But instead of giving diabetes the attention it deserved with an inquiry purely focused on highlighting what is needed to improve outcomes for those of us living with the condition and enhancing the health system to better serve us, we were given an inquiry that conflated two separate and significant health conditions. Something was going to get lost in this. And it seems that is diabetes.
Since the report was launched on Wednesday, a lot of media coverage has focused on one specific recommendation: the sugar tax. That was what was on the front page of The Australian, a segment on the Project and in a number of radio interviews. Also mentioned in this coverage was the recommendation about junk food advertising to children. As you can imagine, the commentary from the community has been pretty horrid and completely misinformed. If ever there was a time for not reading the comments, this is it.
I completely agree that a sugar tax is a good idea and have been saying so for years. I also believe that junk good advertising should be banned completely, especially for children, starting with TV and online advertising and extending to sponsorship of children’s sporting activities. Again, I have been involved in initiatives involving this for years. One of the reasons these measures are important is that they make healthier choices more accessible, which can reduce the risk of people developing obesity. And yes, obesity is a risk factor for T2D. However not everyone who is obese will develop T2D and not everyone who has T2D is obese. Yet this nuance is missed completely with simplistic messaging and grouping the two together.
And this nuance is important. As is pointing out that obesity is also a risk factor for many other conditions as well such as several types of cancer, liver disease, heart attack and stroke, high blood pressure, high cholesterol, osteoarthritis, sleep apnoea, mental health conditions, fertility problems and pregnancy problems. Not only T2D, so why is it included in an Inquiry about diabetes?
I shouldn’t be surprised by the media missing the mark completely, but that doesn’t mean that it doesn’t anger and upset me. Because efforts can be made to try to minimise harm and stigma from misreporting. I was asked to contribute to a media release this week about the AID work and I made it very clear that I would not be involved in anything where messaging could be seen as stigmatising. I provided a copy of language position statements and asked to see the release before it went out to make sure that it all aligned. I pointed out to the PR agency that I would publicly call out any media that came from this release if it was in any way stigmatising about any type of diabetes. Sadly, I don’t think there has been that level of care across PR and media groups. Without that care and attention the stigmatising tropes about diabetes, in particular T2D, are in overdrive.
But it’s not just the media. In the report itself, there is this statement: ‘There is a huge burden being placed on health resources by people with Type 2 diabetes’, a statement that clearly blames people with T2D for needing to use our underfunded, under-resourced, understaffed healthcare system. Absolutely no recognition of non-modifiable risk facts or social determinants of health. More stigma. More misinformation. More throwing people with T2D under the bus. And this impacts on all types of diabetes, whether we like it or not.
I really wish that as we are all tripping over ourselves to highlight this Inquiry report, we also stop to think about the messages about diabetes we are setting free into the world. So far, very little of what I have seen hasn’t made me cringe. Far too much has been stigmatising and harmful. We all have a role to play in ensuring that we do not contribute to diabetes stigma, especially when participating in commentary about and the media circus of a new shiny report being launched.
The #dedoc° symposium kicked off ATTD 2024 in the most powerful way. Four community advocates from across the globe presented on a variety of topics including access to insulin during humanitarian crises, access to diabetes care and technologies in low income settings, accessibility of technology for people with diabetes also living with disabilities, and access to research findings. You can hear the brilliant talks from #dedoc voices Leon Tribe, Tinotenda Dzitiki, NurAkca and Asra Ahmed here.
During the panel discussion, there was an important discussion about how and why it is critical for people with diabetes to be included in all conversations about diabetes. Meaningful consultation is the golden ticket here, and there were some valuable comments and suggestions about how that happens. Someone asked the question about reimbursement for lived experience expertise, an often ignored issue when it comes to people with diabetes being involved in research, programs, committees and anything else that takes our time. Our unique perspective cannot be provided by anyone else, and yet there is rarely budget to cover the costs of our participation. Sadly, it’s not routine to offer payment for our time, instead we are often made to feel that we should be grateful for a seat at the table. It’s worth reminding those who don’t value us in a financial way that WE ARE THE TABLE and without us, there wouldn’t be a place setting for anyone else.
It was clear from the conversation that diabetes advocates – even those sitting on stage at International scientific conferences – find it difficult to ask for their valuable expertise and time to be reimbursed.
I jumped off stage and made a bee line for Jazz Sethi. We do this thing at conferences that I’ve started referring to as the ‘Jazz and Renz conference special’. (You can see previous efforts here and here.) Within five minutes we’d hatched a plan for our next project, and today, we’re so excited to share it. It was clear that we need some ‘Rules of Engagement’ that provided a clear and easy way for people with diabetes and those seeking to work with us to understand not only why engagement and consultation is essential, but why it’s also essential to pay for our time.
It’s not just about reimbursement though. It’s also about recognition for that work in a multitude of ways including being included as a co-author on publications, included on programs giving presentations and having our expertise acknowledged as just as important as all other diabetes stakeholders.
And so, here are some simple guidelines that can be used by people with diabetes when working with organisations, researchers, healthcare professionals, industry and anyone else who wants out expert knowledge. Use them in your discussions with anyone who invites you to be involved in diabetes work. Print them out and take them with you when you’re meeting with anyone running a project or convening an advisory group. Share them in your networks so as many people as possible can use the information to guide discussions about ensuring our value is truly acknowledged. We hope that this will make those discussions just a little easier.
And for those who wish to work with us, have a read. If you still think that our time isn’t worth your budget, or our expertise worth real recognition, then it can only be considered that you are doing the very least to include people with diabetes. That’s tokenism. We’re not here for that anymore.




Disclosure
I was an invited speaker at ATTD 2024 where I presented on the T1D Index in my capacity as Director Community Engagement and Communications in the Global Access Team at JDRF International. I also chaired a session on access to research. ATTD covered my registration costs. My travel and accommodation were covered by #dedoc° where I am Global Head of Advocacy. I chaired the #dedoc° symposium at the conference.