In the lead up to our daughter being born, I was told that it was most likely that she would need to go to the special care nursery immediately after she was delivered because of low blood sugar. This had been the case for most of the dozens of other women with type 1 I’d spoken to beforehand, and I was resigned to the fact that there would not be many cuddles for a day or two.
The reality was a little different. As soon as she was delivered, her heel was pricked and her blood glucose was checked. ‘She’s good to go straight to your room,’ said the paediatrician charged with making sure our precious baby was all okay. He placed her in my arms so I could drink in the beautiful little munchkin
‘No; wait. She needs to go to special care. I have diabetes, remember?’ I said, as I lay on the table being stitched up after the C-section, looking in awe at the wriggling, full-cheeked munchkin who had just been lifted from my body.
‘Her blood sugar is fine,’ the paediatrician smiled at me. ‘Aaron can take her to your room and as soon as you are out of recovery you can join them. Lots of cuddles this morning – skin to skin contact is good for you both! We’ll keep an eye on her and do hourly BG checks to make sure she is okay.’
An hour later, I was stitched up, out of recovery and wheeled back into my room where Aaron was sitting holding our new daughter. He stood up and brought her over to me, positioning her on my chest and I pulled away my hospital gown and her swaddling so I could feel her against me.
With the help of a wonderful nurse, we started to learn how to breastfeed. There in my arms was our daughter. I couldn’t stop staring at her and couldn’t believe she was finally with us.
My endo walked into the room to meet her, and see how I was doing at the same moment another nurse walked in to do the first BGL check. As I held our baby, I cringed at the lancet going into her tiny, tiny heel and the tiny, tiny whimper she made.
I looked at the nurse and saw her turn white. “She needs to go to special care. Now. Her BGL is really low.’
My ever-calm endo, looked at the result. ‘I don’t think that is right. Can you check again? Maybe using Renza’s meter?’
‘No!’ said the nurse, starting to panic. ‘She needs to go right now.’ And she snatched the baby from my arms, put her back in her crib and headed quickly out of the room.
‘Go with her!’ I said to Aaron, but he was already on his feet scurrying after our baby girl.
I was in shock. What had just happened? Our baby had been peacefully snuggling with me, drinking in some of the tiny bits of colostrum she could manage. What was the problem?
In the special care nursery, Aaron watched as the doctors and nurses tried and tried and tried to get an IV line into our tiny newborn baby before they finally decided to just give her some formula.
As it turns out, her BGL was fine. They needn’t have bothered trying with the IV. The meter used on the ward was probably faulty. She could have stayed with me and all would have been okay.
But I wasn’t upset – or surprised – because I understood exactly what I was seeing. This was hypo anxiety from healthcare professionals and I’d seen it before.
When in hospital having my appendix out, a nurse walked in when I was checking my BGL. When she saw the 4.2mmol/l on the meter, she insisted a drink two glasses of juice and eat a sandwich, despite my protestations that I was fine and a few jelly beans would more than do the trick to keep me in the safe zone. She stood there watching me as I forced the juice and food down my throat.
In A&E once, an emergency doctor wanted me to disconnect my pump, because it was sending me low, even though my BGL had been sitting pretty in the 5s for most of the time I was there.
Another time, at work, a diabetes educator jumped up to grab me juice and almost shoved a straw in my mouth when she noticed by CGM trace heading downwards, even though my BGL was still 6 and I had plenty of time to treat before going low.
And it’s not just HCPs. In a meeting once, a senior staffer I’d worked with for over two years asked me if I needed a nurse to ‘help me’ after I excused myself for eating a couple of jelly beans because I was preventing a low. ‘A nurse,’ I said. ‘Why?’ I was confused at what was going on. ‘Because you are hypo. To make sure you are okay.’ And then I was more confused because what possible would have ever suggested that this very easy-to-treat hypo would need the assistance of a nurse?
There is a lot of anxiety around hypoglycaemia. Fear of hypos in people living with diabetes and their loved ones can be paralysing. I know that after a particularly nasty or sticky hypo, I get anxious about lows and I see my loved ones watching me more closely.
But I also work really hard to try to keep some perspective about managing them. And those around me know that keeping calm while I’m low and gently asking if they can do anything is helpful, but panicking is not. Interestingly, no one with diabetes has ever been flustered when they see me going low (nor I when around one of my friends having a hypo).
In each of the situations I described above, I needed to do a lot more to settle and reassure the person panicking than to manage my own low blood sugar. Having to calm down the anxieties of others is not really what I want to do while low.
Unfortunately, low blood sugar is a reality of diabetes for many people. I see it as a short term complication – something I do all I can to minimise, and treat as well as possible – that just needs to be managed. Of course, it can be scary. But doing all I can to keep calm yields far better results: I tend to not over treat and eat the whole kitchen when I am calm.
But what I want to know is why so much anxiety from those around us? If we know that the best way to manage a hypo is calmly, rationally and with measured treatment, why the panic? What are HCPs being told about hypos that send them into a spin so they overreact? And what could be done better to ensure those around us help rather than make things worse when we are low?

Calmly. Quietly.








 Renza: You should consider pretty much everything I ever say to you to conclude with one of those – take your pick.
Renza: You should consider pretty much everything I ever say to you to conclude with one of those – take your pick.

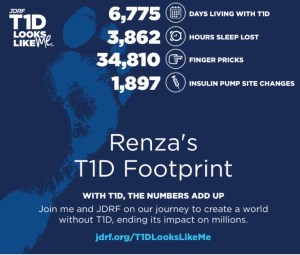


 Get logging for good karma. There’s even an app you can use to make it super easy. (And yes – I’ll be logging before and after I take the pups for a walk!)
Get logging for good karma. There’s even an app you can use to make it super easy. (And yes – I’ll be logging before and after I take the pups for a walk!)






