You are currently browsing the category archive for the ‘Wellbeing’ category.
I’ve been unwell.
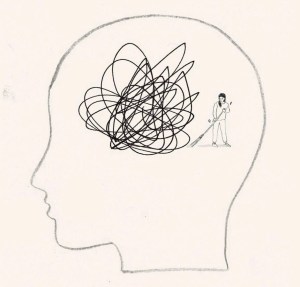
And so, I’ve had time to think. Mind you, I’ve found it difficult to form thoughts properly, thanks to the brain fog that is impacting my attention span and ability to think things through to a conclus…oh look! The leaves on the trees in the garden are changing. I should buy the last plums when I go to the fruit and veg shop, and bake a plum cake. That would be delici… Are mandarins in season yet? Ooh, a puppy!
Anyway, back to trying to focus on what I’ve been randomly and messily thinking about.
On my last day at ATTD in Amsterdam, I wound up with a very weird pain flare that meant I could barely move. I put two and two together, came up with the wrong answer and decided it was thanks to arthritis and spent the day before my flight desperately trying to sleep it off so I would be okay to navigate Schiphol Airport and get myself home. I did make it home, but not without wheelchair assistance at each airport, and in excruciating pain for the entire long trip home.
Turns out, it wasn’t arthritis. It also wasn’t diabetes, but that didn’t stop me from trying to connect non-existent dots.
The day before the paralysing pain flare, I woke at 3am with my Dex alarm wailing. I was low. Very low. For five hours. You know, one of those lows that just won’t quit. One of those lows that simply won’t respond to massive quantities of glucose. I ended up throwing up after force feeding myself jellybeans and guzzling juice from the minibar, which was all just lovely. (And yes – I realised I had some inhalable glucagon with me AFTER the fact … but in my low fog, forgot as I was just trying to stay alive with sugar.)
Of course, I was exhausted when I finally came back in range and felt like I’d been hit by a truck. But sure enough, I got up and had a frantic day at the conference centre, in meetings, giving talks and trying to appear functional while feeling absolutely wrecked.
The next day, when I woke up unable to move because I was in pain, I thought that perhaps it was a result of overdoing things the day before, when I should have perhaps taken the morning off to recover from the hypo and the exhaustion that came with it. But of course I didn’t. Because when have I ever taken time off for diabetes? One time I had an evening black out hypo in a park requiring paramedic attention and I was in at work at my desk by 8.30am the next day. Because why wouldn’t I be? My weird and illogical attitude is that if I was to take time off to recover every time diabetes doesn’t play nicely, I’d be taking hours off each week. No one has time for that. At least, I certainly don’t.
And how very messed up that thinking is. I realise that. And I know what I say to friends with diabetes who tell me about their particularly crappy hypos, or when diabetes is kicking their arse/ass: ‘Take the time and let your body rest,’ I’ll say. ‘You’ve just been dealt a pretty shitty blow to your body and mind. Don’t overdo it,’ I’ll remind them.
And what do they do? They don’t rest. They don’t listen to their body. They overdo it. It’s what we do.
It’s messed up and we keep doing it, even though we know better. Of course we know better: because we give good advice to others. But we then do that ridiculous thing where we think resilience is strength, where actually, resilience would be listening to what our bodies need and then doing it. We ignore symptoms and give ourselves imaginary gold stars for ‘pushing through’.
It took some weird virus that literally hampered my ability to walk for me to take time off work. Sleeping 20 hours a day was all I could manage. But you know what? I should have slept 20 hours the day after the five-hour low to recover too, but of course I didn’t.
Who am I trying to impress by soldiering on as though there’s nothing wrong? What am I trying to prove? Do I think we get extra points in some bizarre Hunger Games-like challenge? Is it that I worry what others will think of me if I say, ‘I need to stop for a bit’? Am I afraid of seeming weak? Lazy? Or am I – twenty-seven years later – trying to live up to the ‘diabetes doesn’t change anything’ line I was fed the day I was diagnosed, even though it changes everything?
I’ve been back home now for two weeks now and really just getting back to regular programming now. On Sunday I was able to stand up for long enough to bake a cake. That was a win. I also was able to walk to our local café – a five-minute walk away – but needed a lift home. Slowly, but definitely better.
I’m not pushing myself – partly because I can’t, but also because I refuse to and that is something that is very weird for me. I’m home this week instead of flying to Bangkok to speak at the IDF Congress – the first time I have ever cancelled a work trip. Usually I push through. Usually I suck it up and pretend all is fine. Because I drank the ‘diabetes-won’t-stop-me’ Kool Aid when instead, I should have recognised that there is no shame in stopping to rest. I need to be better and do better about this. And listen to the advice I would give everyone else. Permission to take time out for diabetes.
This post is dedicated to my darling friend and #dedoc° colleague Jean who also doesn’t know when to stop. Let this be a reminder to put down the Kool Aid!

When the clock ticked over into 2025, I had no intention of even considering coming up with New Year’s resolutions that would shape my new year. But with all that is going on in the world, I’ve given myself permission to reconsider and do all I can to stick to it. And I’m encouraging everyone I know to make the same resolution.
And that resolution is to do a health literacy check-up and to actively pushback against misinformation. There has never been a time when being health literate is more important. I thought that during the COVID years as we received a daily onslaught of misinformation about vaccines, bogus treatments (bleach, anyone?), outright lies (“it’s just a cold”) and conspiracy theories (“BigVax is behind it all”). But how naïve I was. Those days seems like just a warm-up for what is happening today.
I’m in Australia, but I don’t for one moment think we are immune to the madness sweeping the world. But if you are shaking your head and laughing a little when RFK Jr spews his anti-vax, anti-fluoride, anti-science agenda, or Dr Oz uses his latest pseudoscience claim as the foundation for whatever supplement he is selling, you’re not grasping the seriousness of what is going on. Before we Aussies get too smug, we should remember our own backyard isn’t devoid of charlatans, and it’s only a matter of time before someone like Pete Evans is taken seriously in public health discussions. Think I’m over-reacting? He already made a run for the senate. How long before a conservative party sweeps him into their fold?
I think it’s safe to say that we have moved beyond this sort of misinformation being a fringe issue amongst ‘crunchy’ parents, trad wives and ‘wellness’ influencers. And Gwyneth Paltrow.
Health misinformation is deliberate and it’s mainstream, and protecting yourself against it isn’t optional – it’s essential.
Up until now there have been guardrails in place to protect public health. Boards and regulatory agencies have existed to ensure medical safety and provide us with confidence that there are processes in place to determine the safety of drugs, devices, healthcare programs. Guidelines are based on robust and rigorous research and are developed using evidence and expert consensus. (Side bar: Have people with lived experience been involved in these practises? Absolutely not enough. Could this be better? Absolutely yes.)
Critical thinkers understand that science is not static. We understand that science changes as evidence evolves. We also understand that we don’t have to follow guidelines blindly. We should understand and consider them. And then use them to make informed health choices. I repeatedly say this to anyone who questions off label healthcare (my favourite kind of healthcare!): ‘I understand guidelines and learn the rules so I can break them safely’. That’s what being health literate does – it gives me an understanding of risks and benefits to make decisions about my health and what works best for me. And it gives me confidence to spot and push back on misinformation.
Critical thinkers also know that questioning medical advice is not the same as embracing conspiracy theories. It doesn’t mean throwing the baby out with the bathwater as you hastily reject modern medicine in favour of snake oil salespeople. It certainly doesn’t mean denying the effectiveness of a vaccines. And it doesn’t mean trusting Instagram wellness influencers.
More than ever, now is the time to do some questioning – to question who is spreading health information and consider their motives. What are they selling? (Case in point: Jessie Inchauspe who offensively calls herself ‘Glucose Goddess’ while selling her ridiculous ‘Anti Spike’ rubbish as she spreads fear about perfectly normal glucose fluctuations in people without diabetes). And a question that right now should be front of everyone’s mind: What power grab is behind the way someone is positioning themselves as an oracle of health information?
This post is about health literacy in general, but because this blog is called ‘Diabetogenic’ and I have diabetes, most people reading will be directly impacted by diabetes. And if there is any silver lining in this shitshow, it’s this: We’ve been dealing with health misinformation about our condition for decades, so in some ways, we’re probably ahead of the curve. We’ve had to wade through the myriad cures and magic therapies, the serums and pseudo-therapies. And the cinnamon – so much cinnamon! We’ve been standing up for science, challenging misinformation, and ensuring that diabetes health therapies are based on evidence, not fairytales. We’ve expected truth in our healthcare. It’s seemed the normal thing to do. Now it feels like a radical act to be a critical thinker.
We are a crucial point because health is being weaponised more than ever. Someone told me the other day that my lane is diabetes and health, and I should leave politics out of it. It’s laughable (and terrifying) to think that anyone doesn’t understand that health is political. It always has been. And even more so right now. We are seeing in real time political figures (and rich white men who own electric car companies) weaponise health misinformation for their own agendas, and scarily people are listening to them. They are elevating unqualified voices and aligning with conspiracy theorists, giving dangerous misinformation legitimacy. (And if you think that it’s all eerily familiar, you’re right. It’s already happened with climate change.)
Your radical act is to be smarter, to be more critical, to question sources and motives; follow reputable sources, don’t share viral posts before fact checking (Snopes is super useful here). Don’t reject credible advice and information in favour of conspiracy theories. Stack your bookshelves with books by qualified experts (I’d recommend starting with Jen Gunter’s holy trinity – The Vagina Bible, The Menopause Manifest and Blood and Emma Becket’s You Are More Than What You Eat), including lived experience experts who base their healthcare on legitimate evidence. Follow diabetes organisations like Breakthrough T1D (JDRF in Australia) for research updates and community efforts and be smart about which community-based groups you join. If moderators are not calling out health misinformation, I’d be questioning just how the group is contributing to diabetes wellbeing.
We know knowledge is power. But that knowledge base has to be grounded in fact, not fiction. Health literacy is critical because misinformation isn’t going anywhere, and neither are the people pushing it for profit and power. My resolution is to sharpen my critical thinking skills, ask questions, and refuse to let bad science set us backwards and cast a dark shadow over the health landscape. Who knew something so fundamental could be such a radical act?

Colour me unsurprised they couldn’t back up their claim with evidence.
There are different types of burnout. Diabetes burnout, advocacy burnout, and just plain life burnout.
Diabetes burnout rears its ugly head for many of us living with the condition – sometimes starting as diabetes distress before building and building.
Advocacy burnout seems inevitable the more I discuss it with advocate friends. The living with, working in, supporting others with, diabetes becomes a lot. Too much. So much.
And life burnout seems to be inevitable in the fast-paced, never-pause-for-a-breath, always-switched-on lives we live.
When the three collide it’s a triple threat burnout. Welcome to mine.
The white noise hum of diabetes burnout – always there – slowly, but surely had become amplified. It was little things – I was regularly forgetting to bolus when I ate. Not immediately replacing CGM sensors when one fell off. Ignoring making the follow up diabetes appointments I needed to make, the pathology visit I needed to schedule, the supplies stocktake I needed to do to make sure I didn’t run out of anything.
I’ve been hovering on the edges of advocacy burnout for some time and found myself plunged into it earlier in the year dealing with the complexities that played out as I offered my help and support in some volunteer grassroots advocacy here in Australia.
And life burnout suddenly appeared in the form of exhaustion, but an inability to sleep soundly, and a brain fog that I explained away as a perimenopause symptom. Except it was more than that. It was getting to four in the afternoon before realising I’d not eaten a thing all day. And not remembering if I’d showered, or how many days had passed since I last washed my hair. It was a lethargy that gnawed at me all day long.
I focused on plans for a conference in the US, followed by a few days at work headquarters, knowing that it would be a busy and wonderful time, with a lot of interesting work. I could do it. And I did. The conference was excellent. The diabetes advocates there shone so brightly. And every meeting was a huge success.
Smile. Breath. Smile. Breathe.
Until I couldn’t. That moment hit like a tonne of bricks last week.
I’d spent a day in the office at the job I adore, speaking with incredible people doing so much work. I’m inspired daily by the people I work with and learn so much. There were plans set in motion for exciting things to come and I sat in the meeting room I had set myself up in for the day, feeling satisfied and pleased. The workday done, I packed up and stepped out into the street.
And then, a flash, an instant. Suddenly, the pressure bearing down and around on me was so intense and I felt my chest constrict. I struggled to breathe, and my vision blurred. The sounds on the New York streets suddenly seemed to be coming from under layers of concrete, muffled and hushed and yet piercing at the same time. The bright sunlight seared around me, causing me to shield my eyes from the glare.
‘Breathe. Breathe.’ I felt the rising fright of what I know to be a panic attack, and knew I needed to safely just ride it out. ‘Focus. Focus.’ I looked for something I could hold on to. There it was, a small dog, sitting still, staring dotingly at its human seated at an outdoor café, drinking an iced tea. I stood there, slightly hunched over, my arms wrapped around myself, watching this little dog sitting still. I started to count back from 50, getting to 34 before the dog moved, jumping onto its hindlegs, and resting its front paws on its person’s knee.
It was though the crush from the last few months had all converged. I’d tried in small ways to stem it. I limited my time online, muting more terms and accounts that sought to do nothing but argue and inflame. I welcomed the calmness that descended when my Twitter feed was devoid of people yelling about food choices, and when my Instagram feed only showed me the images of my nearest and dearest. I focused my outside of work advocacy efforts to AID access, specifically on the helpers. I threw myself into my job because it allowed me to focus and celebrate the work of others. I amplified the #dedoc° voices and other advocacy to keep my own away from the spotlight. I thought these things worked.
But at that moment, on the streets of lower Manhattan, those attempts didn’t matter or help. ‘But you seemed fine last week,’ said a friend I’d spent time with at ADA a few days earlier. I had been. I was. I thought about how I appear to others. ‘Sometimes, it’s too much. Right now, it’s too much. Forever… it’s too much.’
I felt the uptick in my heartrate. And realised that had been happening constantly. It had happened after the first difficulty with the grassroots advocacy work, and any time I had to face the source of that stress. Sometimes ‘facing’ meant a comment on a LinkedIn post. Sometimes, it meant a somewhat nasty direct message or, even worse, comments that came to me via others. I realised it had happened every time there was some nastiness or other on Twitter. It happened if there was a confrontation of any time around me, even when I wasn’t involved. Anywhere I saw conflict was enough to kickstart an anxiety response.
‘I’m okay’, I said to my friend. And then, ‘It feels too much.’ I felt myself and my mind and the space around me shatter into a million sharp, craggy pieces. And felt my skin being cut against each and every one of those shards.
This is burnout. This is what it feels like. And with it is anxiety and stress and feeling overwhelmed. We all get it to some degree. Diabetes makes it harder. Diabetes advocacy compounds the whole thing even more. Jet lag doesn’t help. Plus there’s a sprinkling of perimenopause over it all. The culmination is a fragility that scares me a bit and leaves me feeling vulnerable. ‘But you seemed fine…’ my friend had said. And I was. Until the burnout took over. And then I wasn’t anymore.
It’s RUOK? day and while I am ready to jump on any worthwhile bandwagon, this one, today, seems especially important. A (non-diabetes) community of which I am on the periphery is grieving today after the death of a much-loved friend and colleague. I’ve been reading beautiful tributes to this person and messages of love and support to their family. I can’t begin to grasp what their loved ones are going through today.
RUOK? is more than a single day. It’s a movement that emphasises the power of human and social connection and having conversations about difficult things. If you’ve not looked at the website, there is advice about building the capacity of support networks (the very foundations of diabetes peer support groups for decades now) and developing skills to have meaningful discussions with someone who might be struggling.
It’s applicable to everyone, including those who may appear to not necessarily need it. Undeniably, it’s very relevant to diabetes. (This article outlines the increased risk of suicide in people with diabetes.)
Diabetes and mental health may be a topic on the agenda at most conferences and we’ve certainly seen an uptick in mental health and diabetes research over the last decade. But the strides that have been made are not enough. The pathway to genuine support and treatment for people with diabetes remains elusive. Simply telling people to seek help falls short when the help they need is not available.
Our peer networks go a long way to offering support, empathy, and love, but we’re not equipped to handle complex mental health issues. While we can assure people that they are not alone and perhaps offer suggestions for where they may find help, this does not go far enough in addressing mental health care, especially in critical situations. Accessing mental health professionals that have knowledge and training to support people with diabetes is what is needed. And it needs to be easily accessible. Easily affordable. Easily available. Right now, that’s not the case.
On RUOK? Day implores us to tap into our social circles and genuinely check in. (Do it, please; just do it). But there is a braider landscape of mental health in the diabetes landscape that needs real transformation. And while it seems unreasonable to add extra burden to those of us living with diabetes – after all, we are already expected to do so much of the physical, emotional, social, and political labour just to get by – community action drives change so often. We have had successful and coordinated community efforts to increase technology funding and access. Is our next frontier turning our attention to increasing funding and access to mental health care for people with diabetes? I know that some diabetes organisations have this in their sights, but without people with diabetes making noise, the campaign is only half-baked. Our voices amplify the urgency of the issue.
Today is just one day, but if RUOK? Day is what provides the gentle nudge to initiate these conversations, it’s a step forward. The tapestry of personal narratives, community connections and shared experiences form the basis of peer support. But not everyone has a safe space where they can share or the people to share with. Sometimes we need to reach out, extend a hand and signal we’re ready to listen. Keep reaching out. Today. And tomorrow. Every time you can.
‘What would the ideal campaign about diabetes complications look like?’
What a loaded question, I thought. I was in a room full of creative consultants who wanted to have a chat with me about a new campaign they had been commissioned to develop. I felt like I was being interrogated. I was on one side of a huge table in a cavernous boardroom and opposite me, sat half a dozen consultants with digital notepads, dozens of questions, and eager, smiley looks on their faces. And very little idea of what living with diabetes is truly about, or just how fraught discussions about diabetes complications can be.
I sighed. I already had an idea of what their campaign would look like. I knew because more than two decades working as a diabetes advocate means I’ve seen a lot of it before.
‘Well,’ I started circling back to their question. ‘Probably nothing like what you have on those storyboards over there’. I indicated to the easels that had been placed around the room, each holding a covered-over poster. The huge smiles hardened a little.
Honestly, I have no idea why I get invited to these consultations. I make things very hard for the people on the other side of the table (or Zoom screen, or panel, or wherever these discussions take place).
I suppose I get brought in because I am known for being pretty direct and have lots of experience. And I don’t care about being popular or pleasing people. There is rarely ambiguity in my comments, and I can get to the crux of issue very quickly. Plus, consulting means getting paid by the hour and I can sum things up in minutes rather than an afternoon of workshops, and that means they get me in and out of the door without needing to feed me. I think the industry term for it is getting more bang for their buck.
I suggested that we start with a different question. And that question is this: ‘How do you feel when it is time for a diabetes complication screening’.
One of the consultants asked why that was a better question. I explained that it was important to understand just how people feel when it comes to discussions about complications and from there, learn how people feel when it’s time to be screened for them.
‘The two go hand in hand. I mean, if you are going to highlight the scary details of diabetes complications, surely you understand that will translate into people not necessarily rushing to find out more details.’
I told them the story I’ve told hundreds of times before – the story of my diagnosis and the images I was shown to convey all the terrible things that my life had in store now. Twenty-five years later, dozens and dozens of screening checks behind me, and no significant complication diagnosis to date, and yet, the anxiety I feel when I know it’s time for me to get my kidneys screened, or my eyes checked sends me into a spiral of fret and worry that hasn’t diminished at all over time. In fact, if anything, it has increased because of the way that we are reminded that the longer we have diabetes, the more likely we are to get complications. There is no good news here!
‘But people aren’t getting checked. They know they should, and they don’t. And some don’t know they need to. Or even that there are complications,’ came the reply from the other side of the table.
Now it was me whose face hardened.
‘Let’s unpack that for a moment,’ I said. ‘You have just made a very judgemental statement about people with diabetes. I don’t do judgement in diabetes, but if you want to lay blame, where should it lie? If you’re telling me that people don’t know they need to get checked or that there are diabetes complications, whose fault is that?’
I waited.
‘Blaming people or finding fault does nothing. That’s not going to help us here. You’ve been tasked to develop something that informs people with diabetes about complications – scary, terrifying, horrible, often painful – complications. Do you really want to open that discussion by blaming people?’
Yes, I know that not everyone with diabetes knows all about complications, and there genuinely are people out there who do not fully understand why screening is important, or what screening looks like. The spectrum of diabetes lived experience means there are people with a lot of knowledge and people with very little. But regardless of where people sit on that spectrum, complications must be spoken about with sensitivity and care.
The covers came off the posters around the room, and I was right. I’d seen it all before. There were stats showing rates of complications. More stats of how much complications cost. More stats of how many people are not getting screened for complications. More stats showing how complications can be prevented if only people got screened.
‘Thanks, I hate it,’ I thought to myself silently.
I spent the next half an hour tearing to shreds everything on those storyboards. We talked about putting humanity into the campaign and remembering that people with diabetes are already dealing with a whole lot, and adding worry and mental burden is not the way to go. I reminded them that telling us again and again and again, over and over and over the awful things that will happen to us is counterproductive. It doesn’t motivate us. It doesn’t encourage us to connect with our healthcare team. And it certainly doesn’t enamour us to whoever it is behind the campaign.
I wrapped my feedback in a bow and sent a summary email to the consultants the following day, emphatically pointing out that I am only one person with diabetes and that my comments shouldn’t be taken as gospel. Rather they should speak with lots of people with diabetes to get a sense of how many people feel. I urged them again to resist using scare tactics, or meaningless statistics. I reminded them that all aspects of the campaign – even those that might not be directed at people with diabetes – will be seen by us and we will be impacted by it. I asked that they centre people with diabetes in their work about diabetes.
But mostly, I reminded that anything to do with complications has real implications for people with diabetes. What may be a jaunt in the circus of media and PR for creative agencies is our real life. And our real life is not a media stunt.
Disclosure
I operate a freelance health consultancy. I was paid for this work because my expertise, just as the expertise of everyone with lived experience, is worth its weight in gold and we should be compensated (i.e. paid!) for it.
Stress impacts diabetes in different ways. And of course, everyone’s response is going to be different.
Before Loop (which now feels like almost a lifetime ago), the effect of stress on my glucose levels was tricky and unpredictable. At times, it would make me high. Other times, I’d be in Hypotown (the town no one wants to visit) for hours, without any respite. The clever Loop algorithm tidies most of that up for me these days.
But when it comes to diabetes, stress doesn’t only impact what I see on my CGM trace. It’s far more than that. Loop can only do so much… Insulin automation doesn’t mean diabetes automation. And it certainly doesn’t mean life automation.
Let me talk about how it’s affected things in the last couple of months …
To some, it might look as though I have become lazy about my diabetes management. I have run out of insulin in my pump more times than I care to admit, scrambling to find my spares bag to refill the canula. I ignore the alerts, silencing alarms and putting the task that needs to be done out of mind.
I’ve let the batteries on my pump and RileyLink wear almost right down. In fact, the batteries have got to the point where they are so crucially low Loop has stopped working. Even the Red Loop Of Doom on my Loop app hasn’t been enough to swing me into action.
I’ve almost run out of insulin. I never do this. Ever. I have a system that works for ordering new scripts to make sure that there is always at least two weeks’ supply, and then back up plans for my back up plans. And yet, there I was, staring down the last few drops of insulin in a penfill. I don’t use insulin pens. I use vials. But I’d run out of vials and was using a penfill that I have for absolute emergencies.
This had become an emergency.
Same goes for pump consumables. I was reduced to searching the depths of my diabetes cupboard and discarded handbags looking for an infusion set, desperately hoping that there was at least one, somewhere, that would do the trick before I had to knock on the door of my neighbour, asking her to tide me over.
This is one part of diabetes burnout for me – the way that I deal with my diabetes tasks. It’s not feelings of resentment that I must do those tasks; it’s not feeling distressed that I must do them. It’s not even feeling a paralysis about doing them. It’s simply not caring enough about them to take the time and energy to engage my brain and actually do it.
I know that when I am stressed, something’s gotta give, and for me, that’s always been doing diabetes.
I cannot tell you how much having automated insulin delivery sweeps up a lot of it. Forgotten boluses get sorted by Loop. Sure, it may take a little extra time and mean a bit of extra time above my upper range limit, but if I don’t engage, Loop will bring me back in range soon enough.
The low-grade nausea I’ve been living with for the last month means that eating is sometimes difficult, but I don’t even need to think about what that means for glucose levels, because Loop mostly does it for me.
And sleep! Sleep the gift that Loop keeps giving has been interrupted, not by diabetes, but by waking stressed. Or, as has happened twice in the last week, with a splitting headache, so painful that the throbbing has woken me from a deep sleep. Pre-Loop, sleep disturbances would wreak havoc with my glucose levels (often because most of the time those disturbances were because of my glucose levels). But now, as I see the upward spike start because I’ve been woken in the middle of the night and glucose is being dumped because apparently, I’m now up and awake, Loop kicks in with an ‘I don’t think so’, and that spike is shut down quickly.
But the nausea is debilitating physically. And being woken in the middle of the night is exhausting. And the stress is leaving me feel a little hopeless all around, to be honest. Teary, emotional, tired. And burnt out.
Many years ago, after a couple of periods of intense burnout, I did a smart thing and found a psychologist to help me. Together, we learnt to identify the triggers that precipitated burnout. This has truly become one of the most powerful tools in my diabetes emotional wellbeing arsenal, because learning when I am heading down the slippery slope of burnout, and realising it’s coming, has meant that I’ve been able to address it before I get so deep into that dark space, it becomes challenging to come back from.
So, right now, I know this is happening. I can feel the stress and the physical manifestation of it, and I can see how it is influencing my diabetes. Today, I spoke with my psychologist – in a way waving a white flag of surrender knowing that I need someone else to come in and help me through this, because I can’t do it myself.
The win is that I’ve seen it and I’ve recognised it. The win is I’m seeking help. The win is that I’ve caught it before I’m plunging to dark depths (I hope).
It’s not a win that I’m feeling this way. It’s not a win that this level of stress has started to affect so much, including my diabetes. It’s definitely not a win that I’ve reached the point where I’m staring down the path to diabetes burnout despite the reason being un-diabetes-related stress.
But that’s how it goes. Diabetes becomes part of it. Of course it does. Because diabetes is always part of it. Always part of everything. Always hand in hand with whatever else is going on. Stress and diabetes leading to burnout. One of the few equations in diabetes that I can count on.
Diabetes and menopause – there are two things that have an image problem! Diabetes’ image problem has been discussed a bazillion times on here and is well documented by others.
And menopause? Menopause is middle-aged women; women who are past their prime and ready to settle down with a pair of slippers and a good book. Women who are a hot mess rather than just hot. Angry old women who are, at best, easily ignored, at worst, are given labels such as the incredibly sexist and derogatory ‘Karen’ thrown at us, especially if we dare demand attention for issues that are important to us. Oh, and we are invisible, apparently.
Well, fuck that. I am none of those things. I am as loud and out there and determined as I have always been. Sure, I like the idea of settling in for the night with a good book and a cup of tea, but I’ve been like that since I was in my twenties. And the anger isn’t new. Being radicalised as a kid does that to you, and I fairly, squarely, and gratefully credit my mother for it.
Turns out that my attention now is being turned to an issue that is one of too little research, too little attention, and too little available information that is relevant, evidence-based and engaging. And that is diabetes and menopause, and perimenopause.
Yes, I’ve written before about before. Missed it? Well, here you go: This time; this time and this time.
If you jump on Twitter now and search the words ‘diabetes’ and ‘menopause’ you’ll find a number of discussions which have been started by people with diabetes who are desperately looking for information to do with the intersection of these two topics. As well as information, people are asking to be pointed to examples of others who have been through it and are willing to share their stories. At the recent #docday° event, the inimitable Dawn Adams from IRDOC gave a rousing talk about why we need to focus more on this issue. (Follow Dawn on Twitter here.)
Here’s the thing: I still get diabetes and pregnancy reminders from my HCPs despite being 48 years old and very clear that having a baby right now (or ever again) is not on my to-do list. Been there, done that, bought the t-shirt and have an almost fully formed adult to show for it!
And yet despite that, I still get reminders about how important it is to plan for a pregnancy, take birth control to prevent it, and make sure that I take folate. Cool. That’s really important information. For women planning to get pregnant (and the birth control bit is important for women looking to avoid it).
But more relevant; more targeted; more person-centred for me is information about perimenopause and menopause.
Just over twenty years ago, when I was looking for information about diabetes and pregnancy, there wasn’t a heap of it. There was, however, a lot of research about it. What we really needed were resources for people with diabetes who wanted information that didn’t look as though it had been written and illustrated in the 1980s. We wanted the evidence-based materials that didn’t scare us. And so, working with other women with diabetes who were the same age as me, and looking for the same sort of information, we made it happen. The diary I published online when I was pregnant added to other stories that were already there. It was hugely reassuring to know that I could find others who were sharing stories that either mirrored my own or suggested the path that mine might follow.
These days, it’s super easy to find stories about pregnancy and diabetes. You don’t need to search too hard to find and follow diabetes pregnancies on Instagram, from pregnancy announcements through to delivery announcements and every twinge, craving and diabetes concern in between.
Less so menopause. Look, I get it. What’s the cute, good news story here? With pregnancy stories, there is a baby at the end – a gorgeous, cooing baby! There is nothing like that with menopause. Despite that, I think there are stories to tell and share. And a community to provide support and lived experience advice.
Right now, there is a chorus of people in the diabetes community who are calling out for this information and talking about the topic. I’m willing to bet that a lot of us were the ones who, twenty years ago, were calling out for decent diabetes and pregnancy info.
I’m not a clinician and I’m not a researcher. I don’t write grants for studies about menopause and diabetes that suddenly put this topic on the research agenda and start to help grow an evidence base. But what I can do is generate discussion and create a space for people to share their stories, or ask for information in the hope that others will answer the call.
The ‘The Diabetes Menopause Project’ isn’t really a thing. It’s a community cry to generate that discussion and some lived experience content. There are some great pieces already out there and I can’t tell you how many times I’ve pointed people to those blog posts and articles. But there needs to be more, and they need to be easier to find.
And so, to start with, here is what I do know is out there. If I’ve missed something, please let me know and I’ll add to it. At least then there is an easy one stop place to find the limited information that is out there. Get in touch if you have something to share.
The Big M – More Taboo Subjects, from Anne Cooper.
Type 1 and the Big-M – a five-part series from Sarah Gatward about her personal experiences of type 1 diabetes and menopause from Sarah Gatward
Managing Menopause and Type 1 Diabetes – also from Sarah Garward, published by JDRF-UK
Menopause + Type 1 Diabetes – Ginger Viera’s writing for Beyond T1
I hosted a Facebook live with endocrinologist, Dr Sarah Price where, amongst other issues, we discussed diabetes and menopause
Research!! This journal article looks at the age menopause occurs in people with type 1 diabetes