You are currently browsing the category archive for the ‘Pumps’ category.
This week, I’ve been at the Australasian Diabetes Congress. By ‘at’ I mean ‘sitting in my home office in lockdown, watching sessions on my MacBook’, because that is what ‘at a conference’ means in the time of COVID.
Today is the final day, and I spent a couple of hours in the technology session, listening to news about the latest and greatest in diabetes technologies, as well as the best way to work with people with diabetes who are using these technologies. I’ll be writing about the latter next week.
Today is all about shiny new stuff!
Big tech news from the Congress was the announcement from Insulet Australia that Omnipod DASH will be available this month, which is fabulous because it means that there is another choice added to the pump market for Aussies with diabetes – and a tubeless pump at that!
The not-so-great news is that Insulet has been unable to successfully negotiate a reimbursement model with the Department of Health. Pumps in Australia are generally covered through private health insurance, and pump consumables subsidised through the NDSS.
This has worked perfectly well to date because pump products have been easily divided into devices (the actual pump) and consumables (infusion sets and reservoirs/cartridges). The Omnipod system is different – it comprises a tubeless pod which is, essentially the pump and consumables. The pod is worn for three days before being discarded. There is a touchscreen ‘personal diabetes manager’ which is used to drive the device. This system simply doesn’t easily slide into the funding model that has worked for the last thirty odd years.
The latest notice from Insulet Australia is that they will now have to go through another submission process, and that will take a further 8 – 12 months. There is no guarantee of reimbursement at the end of this process, but Insulet – and Aussie PWD – are hopeful there will be good news.
Frustratingly, this means that anyone who decides that they really want an Omnipod and want it now needs to purchase it out of pocket, with no subsidy scheme on offer. The price that was announced at the Congress is AUD$400 for a one-month supply. There will be discounts for two- or three-month orders.
In other new tech news, Abbot’s new flash glucose monitor, Libre 2, is very much now available in Australia, and the positive here is that it is already listed on the NDSS for those eligible for the CGM Initiative. Those of us who need to pay out of pocket, the price is the same as for the first-generation Libre. It’s a small win.
Libre 2 has been out and about in Europe for some time now (and Libre 3 is out in limited release in some markets), and has recently received approval for use in the US.
The main difference with Libre 2 is that it alarms when glucose levels are out of range. The wearer will still need to scan over the sensor (either with a mobile phone or reader device0 to see the actual reading, but they will have been alerted to any numbers that are either too high or too low. The great thing is that the alarms are optional, which is great for PWD who prefer their diabetes to be silent.
It’s been described as an evolution rather than a revolution, which is not a negative. We don’t necessarily need every new generation to be a complete and utter overhaul with all new bells and whistles, but it’s always great to see improvements – especially when they are improvements PWD have recommended! I haven’t tried the Libre 2 yet, but will be doing so in the next week or so.
You can find more information about these two new technologies by clicking on the images below.
Omnipod (there is currently very limited information on the site, however that should change in coming weeks.)
Disclosures
Thanks to the Australian Diabetes Society and Australian Diabetes Educators Association, organisers of the Australasian Diabetes Congress for complimentary registration to attend the conference. This gave me access to all the sessions.
I hosted the Australian launch of the Omnipod DASH for diabetes advocates back in May this year, and was paid an honoraria for my time.
Abbott Diabetes Australia has provided me with a Libre 2 sensor to use.
All words here are mine and I have not been asked or paid to write anything you’ve just read.
Last night, my gorgeous friend Andrea tweeted how she had seen someone wearing a CGM on the streets of Paris. When she rolled up her sleeve to show him her matching device, he turned and walked away. ‘Guess you can’t be best friends with every T1D’, she wrote. ‘Diabetes in the Wild’ stories have been DOC discussion fodder for decades – including wonderful stories of friendships being started by a chance encounter, and less wonderful stories such as Andrea’s most recent encounter. I was reminded of the many, many times pure happenstance of random diabetes connection has happened to me.
There was the time I was waiting for coffee and another person in line noticed my Dexcom alarm wailing, and the banter we fell into was so comfortable – as if we’d known each other forever!
And that time that someone working the till at a burger flashed her CGM at me after seeing mine on my arm and we chatted about being diagnosed as young adults and the challenges that poses.
Standing in line, queuing for gelato, is as good as any place to meet a fellow traveller and talk about diabetes, right? That’s what happened here.
And this time where I spotted a pump on the waistband of a young woman with diabetes, and started chatting with her and her mother. The mum did that thing that parents of kids with diabetes sometimes do – looking for a glimpse into her child’s future. She saw that in my child, who was eagerly listening to the exchange. But I walked away from that discussion with more than I could have given – I remember feeling so connected to the diabetes world in that moment, which I needed so much at the time.
I bet that the woman in the loos at Madison Square Garden wasn’t expecting the person who walked in at the exact moment she was giving herself an insulin injection to be another woman with diabetes. But yeah, that happened…
I’ll never forget this time that I was milliseconds from abusing a man catcalling me out his car window, until I realised he was yelling out at to show me not only our matching CGMs, but also the matching Rockadex tape around it. My reaction then was ridiculous squealing and jumping up and down!
Airports have been a fruitful place to ‘spot diabetes’, such as the time my phone case started a discussion with a woman whose daughter has diabetes, except we didn’t really talk about diabetes. And the time another mum of a kid with diabetes was the security officer I was directed to at Amsterdam’s Schiphol Airport. She was super relaxed about all my diabetes kit, casting her eyes over it casually while telling me about her teenage son with diabetes.
The follow up to this time – where I introduced myself to the young mum at the next time who I overheard speaking about Libre, and saying how she was confused about how it worked and how to access it – but not really being all that sure about it, is that she contacted me to let me know that she’d spoken with their HCP about it, had trialled it and was now using it full time. She told me that managing diabetes with toddler twins was a nightmare, and this made things just a little easier.
Sometimes, seeing a stranger with diabetes doesn’t start a conversation. It can just an acknowledgment, like this time at a jazz club in Melbourne. And this time on a flight where we talked about the Rolling Stones, but didn’t ‘out ourselves’ as pancreatically challenged, even though we knew …
But perhaps my favourite ‘Diabetes in the Wild’ story is one that, although I was involved, I didn’t write about. Kerri Sparling wrote about it on her blog, Six Until Me. Kerri was in Melbourne to speak at an event I was organising, and one morning, we met at a café near my work. We sat outside drinking our coffees, chatting away at a million miles an hour, as we do, when we noticed a woman at the next table watching us carefully. We said hi, and she said that she couldn’t help listening to us after she heard us mention diabetes. She told is her little girl – who was sitting beside her, and was covered in babycino – had recently been diagnosed. I will never forget the look on the mother’s face as two complete strangers chatted with her about our lives with diabetes, desperately wanting her to know that there were people out there she could connect with. I also remember walking away, hoping that she would be okay.
Five years later, I found out she was okay – after another chance encounter. I was contacting people to do a story for Diabetes Australia and messaged a woman I didn’t know to see if she, along with her primary aged school daughter would be open to answering some questions. Turns out, this was the woman from Kerri’s and my café encounter. She told me how that random, in the wild conversation made her feel so encouraged. She said that chance meeting was the first time she’d met anyone else with diabetes. And that hearing us talk, and learning about our lives had given her hope at a time when she was feeling just so overwhelmed.
I know that not everyone wants to be accosted by strangers to talk about their health, and of course, I fully respect that. I also know there are times that I find it a little confronting to be asked about the devices attached to my body. But I also know that not once when I’ve approached someone, or once when someone has approached me has there been anything other than a warm exchange. I so often hear from others that those moments of accidental peer support have only been positive, and perhaps had they not, we’d all stop doing it. It’s a calculated risk trying to start a conversation with a stranger, and I do tread very lightly. But I think back to so many people in the wild stories – the ones I’ve been involved in, and ones shared by others – and I think about what people say they got out of them and how, in some cases they were life changing. A feeling of being connected. The delight in seeing someone wearing matching kit. The relief of seeing that we are so alone. The sharing of silly stories, and funny anecdotes. And in the case of that mum with a newly diagnosed little kid, hope.
Today’s post is dedicated to Andrea whose tweet kicked off this conversation in the DOC last yesterday. Thanks for reminding me about all these wonderful chance meetings, my friend.
Last week, I posted this on Twitter:
I take no credit for these numbers or that straight CGM line, or the first thing in the morning number that pretty much always begins with a 5. Those numbers happen because my pancreas of choice is way smarter than me. Actually, in a perfect world, my pancreas of choice would not be outsourced, but what are you going to do when the one you’re born with decides to stop performing one of its critical functions?
Anyway. I should know by now that any time diabetes thinks I’m getting a little cocky or too comfortable, something will happen to remind me not to get used to those lovely numbers.
And so, we have Tuesday this week. I woke up with a now very unfamiliar feeling. I reached over and looked at my CGM trace which immediately explained the woolly-mouth-extreme-thirst-desperate-to-pee-oh-my-god-I’m-about-to-throw-up thoughts running through my head. I found the culprit for that feeling very quickly – a pump with an infusion set that had somehow been ripped out overnight.
I didn’t get a screenshot of that number in the high 20s to share, because my head was down the loo. Ketone-induced vomiting is always special first thing in the morning, isn’t it?
I put in a new pump line, bolused and waited, all while resisting the urge to rage bolus the high away. Because that’s all there is to do, isn’t there? I hoped that just waiting and allowing Loop to do its thing would work, and that everything would settle neatly – especially my stomach which was still feeling revolting.
And as I lay there, I had another feeling that is somewhat unfamiliar these days: the feeling that I absolutely loathe diabetes. Beautifully mimicking the waves of nausea were the waves of my total hatred for this condition and how it was making me feel and the way it had completely derailed my morning’s plans.
I don’t feel like that most of the time anymore, because diabetes so rarely halts me from taking a moment out to deal with it. Hypos are so infrequent, and so easily managed; hypers that need real attention just don’t happen; sleep is so seldom interrupted because of diabetes anymore. Life just goes on and diabetes drones on in the background – annoyingly, but not too intrusively.
But this morning was completely handed over to diabetes to wait it out for my glucose levels returned to range – thankfully with a gentle landing and no crash – and for my stomach to stop lurching. Ketones were flushed and the feeling of molasses-y textured blood running through my veins subsided.
By the afternoon I was feeling mostly human, with nothing more than a slight hangover from the morning. But the feeling of diabetes hatred had been reignited and was flashing through my mind constantly.
A couple of days later, with a full day of decent numbers behind me, there is no physical aftermath of those few hours of diabetes trauma. But there is a whisper of the absolute contempt I feel towards diabetes. It’s always there, I guess. It just had reason to rear its ugly head.
This morning I woke up, got myself organised for the day, headed to our local for our morning takeaway coffee. And then I ripped out my pump line on a door handle.

Which, all in all, seems like a pretty damn appropriate way to celebrate my twenty-second diaversary.
One day I might get good at diabetes. But I guess today is not that day.
Other diaversary posts
Sometimes it feels as though discussions in the diabetes are seasonal. Like clockwork, we see the same conversations happen at the same times. Without missing a beat, almost as soon as a scientific conference is over, someone will comment about how difficult it is for PWD to get to conferences (true, however this year, #dedoc° voices could have assisted a number of the people who were stating that), and then there are discussions about disclosure by PWD who are fortunate to attend, even though pretty much every advocate I know who attends these sorts of things does a stellar job of disclosing.
And of course, the nature of the first big meeting of the year, ATTD, means that there inevitably will be noise about the gap in technology access. And you bet this is a discussion that we need to be having on regular rotation.
After attending my first ATTD, I wrote a piece about the complete and utter dichotomy of being at a conference that was only talking about the latest and greatest in technology while, at the same time, whilst the community was in the midst of its usual Spare a Rose month of fundraising. I struggled to balance the idea that we were talking about automated insulin delivery at the same time as urging donations so people could just get insulin!
Today, I’m revisiting the piece I wrote after last year’s ATTD, where my worlds of diabetes technology and language matters merged, and combined this with the over-representation of those at the super-dooper-tech-y end of the diabetes technology spectrum. (‘Super-dooper-tech-y’ is, obviously, a very technical term.)
I don’t for a moment think that meetings with a strong tech focus should end, or that those who are innovators in technologies should take a seat and let others speak. I don’t believe that at all. I will be forever grateful to the pioneers who continue to push the envelope and make things better for people with diabetes. But I do think that we need to ensure that there is equal attention to those who – by choice or because of their circumstances – are not walking around with an algorithm driving their diabetes.
If we truly believe that all diabetes stories matter, then we need to hear from people doing diabetes in every way possible. Perhaps if we make more of an effort to find and hear those stories, we will stop minimising our experiences, and starr seeing that whatever we are managing to do is truly enough…
DISCLOSURE 1 (for ATTD 2020)
I was an invited speaker at #ATTD2020, and my registration was covered by the conference organising committee. My airfare and part of my accommodation to attend ATTD was covered by Lilly Diabetes so that I could participate in the DOCLab advisory group meeting which took place on Friday, Saturday and Sunday. Other accommodation was covered by DedocLabs (I am an advisor for the #dedoc° voices program) and Novo Nordisk (I am a member of DEEP). I have not been asked to write or speak about any of the activities I attended, or anything I have seen at the conference.
We all do a good job at undermining ourselves at times. We use a four letter word that diminishes what we are doing, and limits the value of our experience and expertise. That four letter word is ‘just’.
In diabetes, we hear it all the time: ‘Oh, I just have type 2 diabetes’ as though it is insignificant and doesn’t have any challenges. ‘I’ve lived with diabetes for just a couple of years’ because we think there is only currency in decades of living with the condition, when really any length of time with diabetes is meaningful.
And we are all about minimising our experience when it comes to the treatment of our diabetes. ‘I just use diet and exercise to manage my type 2 diabetes’ or ‘I’m just on tablets’ or ‘I’m just on injections twice a day’ or ‘I’m just on MDI’. The list goes on and on. And on.
I realised just how ridiculous we have become with this when I heard myself, during a conversation with a fellow Looper, ‘Oh, I just use Loop’. (More on that later…)
At the Ascensia Social Media Summit at ATTD we spoke about this, specifically how there is almost a stigma within the diabetes for those seen to not be using the shiniest and brightest and newest of technologies. It seems that some people almost feel embarrassed if they are not constantly updating their technology toolkit with the most recently launched product.
The idea that anything that we are using today is ‘yesterday’s technology’ is wrong. Blood glucose monitoring can’t be ‘yesterday’s tech’ if it is what most people are using to track their glucose. And syringes and pens can’t be considered the ‘old way to deliver insulin’ when that is how the vast, vast majority of inulin-requiring people with diabetes get insulin into their bodies. Plus, every single one of us using a pump must be able to deliver insulin this way because machines break.
Somewhere in discussions about our treatment technologies, we seem to have forgotten that, actually, not everyone wants to be using the latest kit. And that is okay. There is a spectrum of diabetes technology, and as long as we are on it somewhere and managing our diabetes the way that works best for us, then elephant stamps all around!
There is clearly an over-representation of people at one end of that spectrum dominating on and off line conversations. Spend a couple of hours in a diabetes Facebook group and it would be a reasonable assumption that most people are wearing pumps and CGM. But that’s not true.
And it could appear that DIYAPS is the way to go for most people with T1D, when the fact is that numbers are relatively low. It’s hard to estimate exactly, but there may be somewhere between 2,000 and 3,000 worldwide how have ‘built their own pancreas’. That is just a drop in the type 1 diabetes ocean.
It’s fantastic for those of us interested in this technology to be able to (virtually) congregate and talk amongst ourselves. I learn so much from my peers in these groups – just as I have with all aspects of life with diabetes. The lived experience continues to trump any other way of learning about diabetes.
Of course, that doesn’t mean that we shouldn’t be talking about technology used by limited numbers. Of course we should. We want others to know about it so they can make an informed choice about whether it may be right for them. We want our HCPs to know about it and to support those of us using all sorts of technologies and treatments.
Where it becomes problematic is when there is the misconception that this is the norm. Or when those not using the newest technology feel that they are wilfully doing diabetes the ‘old way’. It’s unfair to think for a moment that those who are not using the tech ‘don’t care’ enough about themselves – especially when decisions are made based on a very good understanding of what is available and what they have decided works best for them.
So, back to my ‘Oh, I just use Loop’ comment. It was directed to someone far more technologically advanced than me; someone who runs all sorts of other programs alongside their DIYAPS. They generate lots of reports and make lots of changes and seem to have far more bells and whistles than I even knew were available.
I nodded as they told me all they were doing and then, when they asked me how I manage my diabetes, I answered that I just use Loop. I heard myself saying it and stopped and corrected myself. ‘I mean…I use Loop. It works for me. Perfectly.’
We don’t need to make excuses for doing diabetes our own way. If we truly have choice (which I know is not always the case), and we have made the choice based on what we believe to be the best possible treatment and technology for us at that moment, then surely that’s a great thing. We shouldn’t ever be made to feel less committed to our own health and wellbeing. That’s not how it works.
DISLCOSURE 2 (for ATTD 2019)
I was invited by Ascensia to co-chair the Diabetes Social Media Summit at ATTD (#ATTDDSMS). I did not receive any payment or in-kind support from them for accepting their invitation. I have co-written a piece for the blog, however this was not edited (apart from inevitable jet-lag-induced typos) and all words are those of mine and the piece’s co-author. You can read that piece here.
Last year, I was invited to the Australian launch events of two insulin pumps. Within a month of each other, the YpsoPump and Cellnovo pump were introduced into the Australian market: a market with a huge appetite for something new. Although Cellnovo had launched softly the previous year, the Australian distributor seemed to be increasing their business and had the pump’s inventor, Julian Shapley, in the country to give a presentation and answer questions.
At both events, we were wined and dined, and the latest bells and whistles of these two new offerings were confidently and excitedly shared with us. I listened carefully, keen to hear not only about the technical specifications, but also about the customer service that would be offered to those choosing these devices and their plans for the future. I’ve learnt over the years that reading glossy brochures only gives one part of the overall picture of using a particular device, so I was looking forward to asking those questions that give a much better idea of what is going on.
At some point during each of the events’ proceedings, I asked the same question. I wanted to know how these companies were safeguarding from these devices being launched on the market with great fanfare only to see them disappear after people had started using the very products in front of us.
Of course, I was assured and reassured that the companies were here for the long-haul and that they were future-proofing themselves by insuring they were preparing for the technology we all expect. Closed loop systems were coming; integration with CGM was an almost done deal; their algorithms would be better, smarter than anything we had seen before. And yes, they absolutely understood the concern I was expressing at the thought that just as quickly as their device had won our hearts and minds, it would disappear from market altogether. Of course, of course, of course that was not going to happen and I shouldn’t for a minute even think that was how things would turn out.
I listened. And I believed them.
Last week we heard that Cellnovo was ceasing production of its pump and all current users would be transitioned onto different devices. This played out over a couple of days. The first announcement was that Cellnovo was going into administration, but I wasn’t ready to shut the coffin lid just yet – we’d seen that happen before. But then, a mere day or two later, the announcement came that all manufacturing and commercial activities would cease, and that no new PWD would be started on Cellnovo products. Coffin. Nailed Shut.
Let’s put aside any opinions of the Cellnovo pump, because that’s not what this is about. I know there were some people who really weren’t fans of the device. My limited interaction with it left me interested, but not keen to slap one on my upper arm and call it my new pancreas. But I know some people who love it and have found it to be the right insulin delivery device for them. My diabetes; my rules and all that.
I also know a number of people who started using Cellnovo as their first pump. In Australia it was the closest thing we had to a ‘patch pump’ and they liked the idea of not having to deal with centimetres of tubing. When I wrote that Cellnovo would be launched here, I had a number of people reach out in great excitement. With Omnipod repeatedly stalling getting through our funding model, this was as good as they were going to get to the device they thought would be best for them.
And so, Cellnovo has won the heart and minds of some people. Just as mine were won over by the Cozmo and Animas pumps. And when they are taken away from us, our hearts break a little.
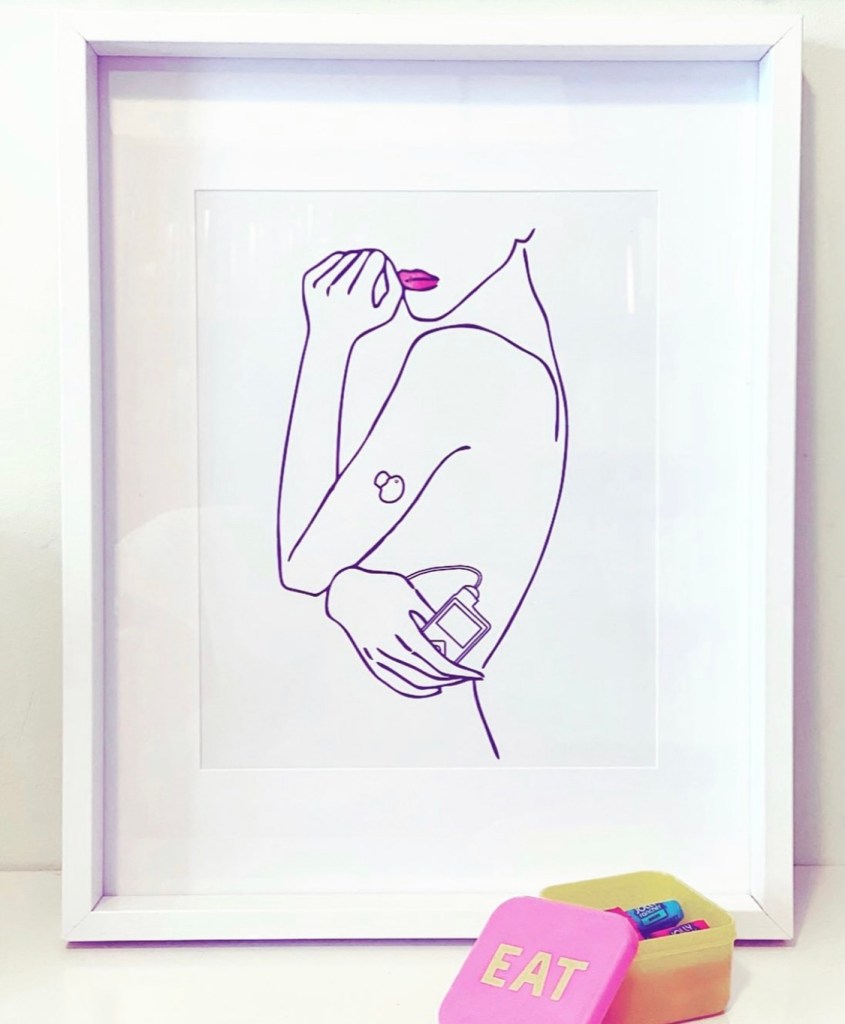
We learn to tolerate and accept – and sometimes even love – these devices. I wear mine as close to my heart as I possibly can, hearing it gently whir as it delivers insulin, sometimes in perfect time with my heartbeat. We do what we can to make them fit with us seamlessly. We know they will never really be part of our body; but we do what we can to work with and around them.
There is nothing and there is no one who I have ever been as literally attached to as the devices that are connected to my body 24/7 for the last eighteen years. I have loved them and hated them in equal measure as each day I try to accommodate them as best I can while at the same time appreciating and acknowledging what they do for me. And I hear this from others who have been wearing insulin pumps (and other diabetes devices) – some for years, some far more recently.

So, with this in mind – and this is something many of us have written and spoken about – and what played our last week, the almost cavalier attitude to my question at the event last June has left a sour taste.
Let me be clear here: this isn’t directed to the team at Medical Specialties Australasia (the Australian distributors of Cellnovo). They have been nothing but professional, friendly and approachable, and from the first time I met with Aaron Crook, it was clear that they were keen to make a success out of things and were pleased to be offering more choice to PWD in Australia. It’s possible they only found out about all of this a short time before the announcement was made. And really, it isn’t necessarily about Cellnovo. They are just the latest in the casualties of medical devices, and now join the ranks of Cozmo, Animas and Asante pump and the Navigator CGM. I am sure that they never wanted this to happen.
And yet, it has.
Of course, the closure of a business leaves a mess, and many casualties in its wake, but perhaps those that will feel this the most personally is PWD – the people who have come to rely on these devices to survive. We are already doing all we can to live with a condition that demands so much. We struggle to find what works for and alongside us and when we do, we want to keep it forever. Our own pancreas already decided to stop working; having to contend with the one we chose as its replacement disappearing as well seems more than just a little cruel and unfair.
Disclosures
I have none that are relevant to this post. My travel and accommodation for both launch events were covered by MSA and Ypsomed and were declared at the time.
I never thought I’d be one to think about back-up plans the way I do now. A few years ago, I remember being extraordinarily proud of myself as I wrote this post about my diabetes spares bag. And then a couple of years ago, I thought I was remarkable and quite brilliant at being able to easily manage when I got to work and realised my insulin pump hadn’t made it with me. I thought I had every contingency sorted and was fabulously good at diabetes. Give me a medal, please.
But in the last six months or so, I’ve come to see I’m not quite as prepared as I thought. I probably should point the finger right now at David ‘Bionic Wookiee’ Burren for this. He has highlighted holes in what I thought was a well-planned strategy a number of times (‘What’s your RileyLink Bluetooth address, Renza? You don’t know? You should.’), shaming me into wanting to do better, and really making me question all my life choices at the same time.
Back-up planning has been covered in both the Australian and European Social Media Summits hosted by Ascensia (disclosure at the end of this post) and it is interesting to see that the level of organisation and preparation varies so much in those of us living with diabetes.
Some people have thought out every possible contingency and have a plan for each one. Others have a fixed idea about what might go wrong and have made accommodations for those (that’s me). And others figure that it will all work out and the diabetes gods will sort it out.
I guess that personality type comes into how well-equipped we all may be. Some of us have a far more lackadaisical approach to planning for the apocalypse than others. But I do agree that it never hurts to be prepared or to consider things that may never have entered your mind before.
So here are some things that I have learnt in recent times that have completely changed the way that I think about my back-up planning.
It’s not just about kit (1). It’s all very well to have back up for what happens if (for example) your pump dies, but if that means returning to MDI until a replacement can be delivered, actually knowing how to do MDI is important. (Bless my endo who always asks if I need any long acting insulin ‘just in case’. She gave me some in-date long acting insulin and we had a discussion about what doses would look like after I proclaimed ‘It’s been 18 years since I gave myself a dose of long acting insulin. And it was Protophane. I have no idea what I am doing.’Lovely endo didn’t even roll her eyes at me when she walked me through exactly what I’d need to do to ensure my basal dose was right and the timing of the injections.)
It’s not just about kit (2). Look – my back up plan to my pump dying is another pump. I have a couple in the diabetes spares cupboard and always travel with one. But I don’t carry one around with me on a day-to-day basis. If I was a couple of hours from home and my pump died, I’d need to know what to do in the meantime. Again – it’s been 18 years since I was on MDI, but I always have a spare syringe and insulin with me so I can bolus until I get hooked up again to a working pump. My injection technique is scratchy – very scratchy, but in a pinch, I can manage it. There’s nothing wrong with asking for some re-education on something for which you may be a little out of practise.
Apparently my long-held belief that the DOC is my back-up plan is not actually adequate, because who is going to be able to provide me with insulin/pump consumables/spare pump/battery/RileyLink at 3am when things like to go wrong. (This is despite the success of the whole Pumpless in Vienna story.)
Equally, having a neighbour with type 1 diabetes two doors down is great when I need a Dexcom sensor at breakfast time. But it would probably stretch and test the neighbourly spirit if I woke her and her family in the middle of the night because I desperately wanted my loop to turn back to green and needed a sensor to do that.
I need a back-up of EVERYTHING I use if I want to be able to seamlessly manage any issue that comes up. With Loop that means a spare Loopable pump, a spare Riley Link, a spare G5 transmitter as well as all the necessary consumables. That takes expense as well as organisation.
CABLES!! They need to be part of my back up plan. I was at a conference last year somewhere (can’t remember where) and remembered as I was about to sleep that I’d forgotten the charger to my RileyLink. And just last month didn’t charge it overnight, meaning that my Loop turned red while I was at work and I was unable to do anything until I got home. Carrying the right charging equipment for all devices is important.
But! If I don’t have all these things, I need to ensure that I have a suitable, easy and fully ready-to-go option that will get me through until I can assemble all required to return to normal service.
When your back up plan becomes someone else’s back up plan, you need to do something about it. Case in point: at the DOCDAY event at ATTD, a friend leaned across the table and asked me if I had a spare battery for her Loopable pump. Of course I did, because there is always at least one in my spares bag. I handed it to her and made a mental note to pick up some more AAA batteries next time I passed a convenience store. Of course, I forgot all about it until Loop started complaining and that the battery was running low. Down to 4% battery and starting to feel a little nervous, I found a tiny little store in a backstreet in Brussels, crossing my fingers as I walked in that there would be a stash somewhere of what I needed. There was and I changed the battery just as my Loop app was showing 0% battery.
Beating ourselves up about our perceived or real lack of planning is unnecessary. As Sophie, one of the participants at #ATTDDSMS, said: ‘Life gets in the way.’ And it does. I challenge anyone not living with diabetes to do their normal life, live with diabetes and not only think about all the ‘just-in-case’ scenarios, but also prepare for each and every one of them.
But mostly, what I have come to see is that the point of a back-up plan is for it to be smooth and simple, with as little disruption to our day as possible. A plan that requires a cast of thousands, hours of travel, is insanely complex and relies on a number of external factors that are potentially beyond our control is not really going to make executing our plan all that easy, or give us peace of mind. And that’s a big part of what this is all about – feeling confident that we can manage whatever gets thrown at us.
That is, after all, the nature of this condition we live with.

DISLCOSURE
I attended the ATTD conference in Berlin. My (economy) airfare and part of my accommodation was covered by DOCLab (I attended an advisory group meeting for DOCLab), and other nights’ accommodation was covered by Roche Global (I attended the Roche Blogger MeetUp). While my travel and accommodation costs have been covered, my words remain all my own and I have not been asked by DOCLab or Roche Global to write about my attendance at their events or any other aspect of the conference.
I was invited by Ascensia to co-chair the Diabetes Social Media Summit at ATTD (#ATTDDSMS). I did not receive any payment or in-kind support from them for accepting their invitation. I have co-written a piece for the blog, however this was not edited (apart from inevitable jet-lag-induced typos) and all words are those of mine and the piece’s co-author. You can read that piece here.
ADATS on Friday was a great day of diabetes technology and treatment advancements.
There was a lot about automated insulin delivery (AID) systems, which, when you think about it, is really what is at the cutting edge of available diabetes therapies in 2018. David Burren, the Bionic Wookiee, gave a keynote on his experience using DIYAPS and why it works for him. And smart endocrinologist Dr Barbora Paldus gave what I heard was a fabulous talk about different AID systems, including what is coming onto the commercial market as well as DIY systems, and providing details (using terminology that made sense to everyone!) about the different algorithms. And fuzzy logic. I’m so annoyed I missed her talk, but it was on at the same time as the session I was chairing (and it’s bad form for the chair to leave the room to go to hear other speakers).
Before going any further, let me say this – not as an statement of tokenism, but as absolutely heartfelt and something I believe one hundred percent. We can talk about systems that automate insulin delivery with the aim to improve diabetes outcomes, but until these are affordable, accessible and available for everyone who wants to use them, we must acknowledge that these technologies will not be able to be used by most people with diabetes. Everyone ‘working in diabetes’ has an obligation to work towards improving access and affordability to minimise the ‘haves’ and ‘haves not’ landscape that we are already seeing, and will see even more in the future.
I chaired a session that focused on the current MiniMed 670G system trials underway in Australia and then hijacked the panel discussion in the afternoon about the topic because the consumer rep. had to leave early. So, where are we with approval for this system (and how long before lucky people can get their hands on one)? Well, the pump is now approved through the TGA, however is not being provided to PWD yet. The new sensor has not received approval yet, and the system as a whole has not either. Medtronic Australia is saying that they are hoping it will be available by the end of the year. The approval process is out of their hands, but I know they are working super hard on their end to get this to PWD as soon as they can.
I have spoken with a few people who have done the trial here in Australia. We need to remember that trial conditions are often not ‘real life’ conditions, so what I am writing about today does not necessarily reflect the experiences of people using the 670G every day and outside of trial conditions. (The system has been launched in the US and there are lots of stories online from people who have chosen to use this system and I would encourage anyone thinking about using it to search for and find what they have to say.)

Research guinea pig and 670G study participant, Leanne Foster.
The session last Friday was comprehensive in that it included presentations from HCPs in the private and public sectors, adult and paediatric settings, a dietitian, and (thankfully) a psychologist. For me, the highlight was hearing from self-proclaimed research guinea pig, (and friend for over fifteen years) Leanne Foster, who has been a long time diabetes technology study participant and was involved in the study.
From listening to the details of the study design, this was not trial for the fainthearted! There were significant demands placed on participants, and expectations were high. To be clear, participants were not given the system, provided with a bit of training and sent on their merry way to simply live alongside the device back in their everyday world. There was a lot of logging, counting, device wearing (not just the pump and CGM that make up the 670G system).
I think it is important to mention this, because one of the themes that was repeated by several speakers was that for many participants, their own burden of diabetes – how much they thought about their diabetes and what they were required to do – increased while using the system on the trial.
It is also important to mention that this is a first generation device. The system that will be launched here is likely to be the same as the one in the US, yet there have already been more sophisticated and aggressive algorithms developed and tested as part of this trial.
While possibly unfair, it is impossible to not compare experiences of people using the 670G and DIYAPS, because these systems are endeavouring to do the same thing: automate insulin delivery, increase TIR, reduce what the PWD is required to do.
And there were some things that struck me as really widening the gap between the two systems.
Firstly, the concept of added burden was astounding as my personal diabetes burden is the lowest it has ever been in the twenty years I’ve lived with diabetes. Since Looping, I think about diabetes far less than I did beforehand.
That burden is not only applicable to PWD. Many of the HCPs who presented said that they found themselves required out of hours significantly more with people using the 670G. I have not once called my HPC about any diabetes-related matter in the last 15 months I’ve been Looping. Obviously, I wouldn’t be contacting her if there was an issue with the system, but I’ve not contacted her for any general diabetes trouble-shooting that would result in me making changes to any of the settings on my tech.
There was a lot of talk about the 670G system ‘booting out’ of auto mode, meaning that automated insulin deliver doses stop, instead going back to the fixed basal rates set in the pump. This happened every day for many people; several times and for a number of hours at a time. I can say that in my experience, my system loops continuously. There are extremely rare times where my green circle turns red, and the pump reverts back to delivering what is set as my basals. But I am always able to troubleshoot by following a few basic steps and Loop will inevitably return to green.
One thing that struck me, was the number of times we heard about the system struggling to cope with the day-to-day lives of the trial participants, and the only way around that was for them to amend their behaviour. There was one moment that had me sitting there in disbelief when I heard the example of one trial participant who was having recurrent lows overnight and the only way to remedy that was for them to have 10g of carbs before bed. Suddenly, I was thrown back to 1998, being on Protophane and Act Rapid, and the only way I could keep horrid night-time lows at bay was to have a glass of milk with corn powder before bed. (Anyone else do that?)
The very idea that new devices being developed will require PWD to change their behaviour for said device to ‘cope’ with our real life is astonishing! This is, without a doubt, a step backwards in my mind. I know that my experience of Loop is that it has easily been able to adapt to my incredibly un-predictable life that includes far too much travel to different time zones, a varied and sometimes erratic diet and days where I have walked 30,000 steps with others where I’ve been horizontal for most of the day. I haven’t had to modify my behaviour in any way to please my Loop, and I’m not sure I would be so enamoured by it if I did.
What is definitely not a step backwards however – in fact it’s a monumental leap forward – is the potential of this technology and technology like it. As a convert of automated insulin delivery systems, the idea that people will be able to soon access devices that commercially available, under warranty and supported by the company’s customer service is only a great thing. Not everyone wants to build their own system, not everyone is comfortable using a DIY system, especially if they don’t feel they have complete support of their HCPs. Once the 670G becomes available, many of the concerns PWD have will be alleviated. Adding choice is only ever a good thing.
But perhaps the most telling sentiment about how the technology impacts on real life came from Leanne. She loved the idea and experience of automated so much (even with all the disclaimers of the trial requirements) that when she was forced to hand back the 670G system when she finished her part of the trial, she as having none of it! After begging to keep hold of the system (which she knew simply could not happen), she had everything ready to go to build her own DIYAPS and has happily joined the Loop family for now. The capabilities of the 670G technology – the automation and the results – such as the improved sleep – were too much of a good thing and she was not prepared to go back to what she had beforehand. And THAT is telling.

Automated insulin delivery panel. L-R: David O’Neal, Sue Wyatt, Kerryn Roem; Jane Speight, Tim Jones, Spiros Fourlanos, me, Jane Holmes-Walker, Melinda Mus
Disclosure
My flights from Melbourne to Sydney were covered by the National Association of Diabetes Centres (NADC), the organisers of ADATS. I am on the organising committee for the conference.
I am not involved in the Medtronic MiniMed 670G trial. I have worked with and consulted for Medtronic on other projects.