You are currently browsing the category archive for the ‘Healthcare team’ category.
Sometimes, I’m a lousy person with diabetes (PWD). I am thoughtless and unclear about what I need, have ridiculous expectations of others – and myself, and am lazy. But I’m not always like that. And I think I know what I need to do to be better.
Being a better PWD is about being true to myself. It is also about reflecting on exactly what I need and I hope to get it.
- I need to remember that diabetes is not going away
- I need to remember that the here and now is just as important as the future
- I need to remember that I don’t have to like diabetes, but I have to do diabetes
- I need to remember that the diabetes support teams around me really only have my best interest at heart, and to go easy on them when I am feeling crap
- I need to empty my bag of used glucose strips more frequently to stop the strip glitter effect that follows me wherever I go
- I need to remember that it is not anyone else’s job to understand what living with my brand of diabetes is all about
- I need to remember that the frustrating and tiresome nature of diabetes is part of the deal
- I need to be better at changing my pump line regularly
- I need my diabetes tasks to be more meaningful – quit the diabetes ennui and make smarter decisions
- And I need to own those decisions
- I need to see my endocrinologist
- I need to decide what I want to do with my current diabetes technology. There is nothing new coming onto the market that I want, but what about a DIY project to try something new? #OpenAPS anyone…?
- Or, I need to work out how to convince the people at TSlim to launch their pump here in Australia
- I need to check and adjust my basal rates
- I need to do more reading about LCHF and decide if I want to take a more committed approach or continue with the somewhat half-arsed, but manageable and satisfactory way I’m doing it now
- I need to remind myself that my tribe is always there and ask for help when I need it.
- I need to make these!
And being a better PWD is knowing what I need from my HCPs and working out how to be clear about it, rather than expecting them to just know. (I forget that Legilimency is not actually something taught at medical school. #HarryPotterDigression)
So, if I was to sit down with my HCPs (or if they were to read my blog), this is what I would say:
- I need you to listen
- I need you to tell me what you need from me as well. Even though this is my diabetes and I am setting the agenda, I do understand that you have some outcomes that you would like to see as well. Talk to me about how they may be relevant to what I am needing and how we can work together to achieve what we both need.
- I need you to be open to new ideas and suggestions. My care is driven by me because, quite simply, I know my diabetes best. I was the one who instigated pump therapy, CGM, changes to my diet and all the other things I do to help live with diabetes
- I need you to understand that you are but one piece of the puzzle that makes up my diabetes. It is certainly an important piece and the puzzle cannot be completed without you, but there are other pieces that are also important
- I need you to remember that diabetes is not who I am, even though it is the reason you and I have been brought together
- And to that – I need you to understand that I really wish we hadn’t been brought together because I hate living with diabetes
- I need you to remember that I set the rules to this diabetes game. And also, that there are no rules to this diabetes game
- I need you to understand that I feel very fortunate to have you involved in my care. I chose you because you are outstanding at what you, sparked an interest and are able to provide me what I need
- I need you to know that I really want to please you. I know that is not my job – and I know that you don’t expect it – but I genuinely don’t want to disappoint you and I am sorry when I do
- I want you to know that I respect and value your expertise and professionalism
- I need you to know that I hope you respect and value mine too.
And being a better PWD is being clear to my loved ones (who have the unfortunate and unpleasant experience of seeing me all the time – at my diabetes best and my diabetes worst) and helping them understand that:
- I need you to love me
- I need you to nod your heads when I say that diabetes sucks
- I need you to know I don’t need solutions when things are crap. But a back rub, an episode of Gilmore Girls or a trip to Brunetti will definitely make me feel better, even if they don’t actually fix the crapness
- Kid – I need you to stop borrowing my striped clothes. And make me a cup of tea every morning and keep an endless supply of your awesome chocolate brownies available in the kitchen
- Aaron – I like sparkly things and books. And somewhere, there is evidence proving that both these things have a positive impact on my diabetes. In lieu of such evidence, trust and indulge me!
- I need you to know I am sorry I have brought diabetes into our lives
- I need you to know how grateful I am to have you, even when I am grumpy and pissed because I am low, or grumpy and pissed because I am high, or grumpy and pissed because I am me.
Yesterday, I had my annual eye screening. In an endeavour to calm me as much as possible from the anxiety I feel about this annual check-up, I made plans so that it would be the same as my check every year. My dad drove me there, sitting in the waiting room while I faced my fears in the doctor’s office.
I have been going to the same eye specialist centre for 15 years. I’ve seen the same ophthalmologist the whole time and his orthoptist has been the same absolutely delightful woman. She does a super job of calming me down, checking my vision and eye pressure and popping in the dilating drops. And then she sends me off to see her boss so he can have a look at the back of my eyes.
‘The main event’ part of my appointment is always fairly similar and I am fine with that. I know what to expect, I know the order of things and I know that I will have an opportunity to talk about anything concerning me.
We start with my ophthalmologist asking me how I have been and what has changed in my life over the last 12 months. I mentioned that I had changed jobs and we had a chat about that for a moment.
Then he asks if there have been any changes with my diabetes in that period and is always pleased (as am I!) when I report on the mostly boring nature of my diabetes. At this point, he usually asks about my family and any recent travels.
And then, the eye exam. The lights go out, I rest my chin on the contraption and he spends a good 10 to 15 minutes having a look at my eyes, explaining what he is looking at, what he is looking for and, most importantly to me, what he can see.
Or – what he can’t see. I am always hoping that he can’t see any diabetes-related eye disease.
‘Remind me how old you are, Renza,’ he said as he turned the lights back on.
‘I’m turning 43 at the end of the month,’ I said, blinking furiously as my dilated pupils tried to get used to the suddenly bright overhead lights.
‘And you’ve had diabetes for 18 years, right?’ he asked.
‘Eighteen and a half…,’ I said.
‘There is absolutely no diabetes-related anything going on in your eyes, Renza. It is all good news from me. You should be really pleased.’
‘I am,’ I said, nodding. I could feel my breathing starting to return to normal, unaware until that moment that I’d been holding my breath.
‘Okay. So…I’ll see you in a year. Of course, come back sooner if there are any changes. But first, is there anything else you wanted to mention?’
‘Oh – yes!’ I suddenly remembered that I had written myself a note in my phone. ‘I have noticed that my eyes have been really watery lately – maybe in the last couple of months. I can’t go outside without tears streaming down my face. It’s a little better if I am wearing sunglasses, but not always.’
‘Let’s have a look,’ he said. ‘It could be a blocked tear duct.’
‘Wait – what are you going to do…?’ Panic was setting in again!
‘Just tilt your head back for a second and I’ll pop some drops in first. And then I’ll do what I need to do.’
I knew that it was not the moment to ask exactly what was going on. I also knew that he has been my eye specialist for 15 years and knows me and my anxieties. And I also know that I trust him completely! I could hear paper rustling – the sound of something sterile being freed from its package.
‘Renza, I want you to look right up over your head for a second.’ At that point, I saw the syringe. ‘Okay – in a second, you are going to feel some saline running down the back of your throat. Nothing to worry about.’
And at the moment I tasted the salt I realised that THERE WAS A NEEDLE IN MY EYE. AND I WAS AWAKE. And I was not screaming. Or in any pain.
‘That one is fine,’ he said. ‘Let me check the other one.’ And he repeated the procedure, again announcing all to be okay. ‘It’s all fine – nothing to worry about at all.’
‘Great,’ I said. ‘Um…did you just stick a needle in my eye?’
‘I will never say,’ he said, smiling at me.
‘I think we need to acknowledge this new phase of our relationship. I feel I have really grown as an eye patient.’ I said as I gathered up my bag. I thanked him for his time – but really I was thanking him for the awesome ‘report’ and the lovely way he deals with me.
‘I’ll see you next time, Renza. Everything is looking really good.’
I walked out of the room. My dad looked up from the magazine he was reading and stood up. ‘All okay?’ he asked. I nooded. ‘Told you!’ he said – just like he always does.
I smiled. ‘Guess what? I just had a needle stuck IN MY EYE.’ I told him. ‘Did you hear me? A NEEDLE STUCK IN MY EYE.’
I settled the account and made an appointment for the end of next year at the front desk and we got into the elevator. ‘I just had a needle in my eye,’ I said, this time quietly and mostly to myself.
‘And my eyes are all clear.’
We walked to the car. All done for another year.

Pupil still slightly dilated. But an all-clear from the ophthalmologist.
Today, I just want to follow up a little about one of the points I wrote about yesterday in my post about the event I attended on Tuesday evening about diabetes-related foot complications, specifically this point made my A/Prof Ramon Varcoe:
He explored how we make people with diabetes know this technique for saving limbs is available, and said that it is really, really important to inform PWD about it so that they can ASK for it and not just accept a diagnosis of requiring an amputation. He said that this was the group that could really drive change here, by demanding that they have the best treatment possible.
This had me thinking long and hard. I agree with A/Prof Varcoe here, but that is not really a surprise. I am so much about consumer-led healthcare, that I dream about it (sad, but true).
Mostly, I thought about it in context of my own diabetes care and how it has happened that I am such a DTech nerd. I decided after about two years of living with diabetes that I wanted to use an insulin pump. I really just could not get the hang of the MDI situation I had been put on at diagnosis and was the living embodiment of why Protophane was referred to as Protopain.
I went to an information session and heard a women speaking about how much she loved using an insulin pump and what a difference it had made for her quality of life. Afterwards, I spoke with her and by the end of our chat, was convinced. I wanted one of those! (Impressionable little thing, aren’t I? #MarketersDream) This woman would become my pump trainer and the only diabetes educator I have ever seen.
At my next endo appointment, I marched in with the research I had done, the questions I needed answered and an expectation that by the end of the consultation, I would leave with details of how and when and where I would be getting my pump. Ha, the naivety!
My endo was absolutely not keen for me to take the pump road, ‘You’ve not had diabetes long enough,’ he told me, which confused me no end, because it already felt like a lifetime. ‘I think we should talk about this again after you’ve had diabetes for about 5 years. Yes?’
Well, no. That was the last time I saw him. I spent the next six months endo shopping until I found one that (I was promised) would agree to helping me on a way to a pump. I walked in and made it very clear why I was there and he nodded straight away. ‘Yep – we can do that,’ and picked up the phone. And about three months later, I was a pumper. This particular endo and I parted ways not long after because I needed someone who was far more expert in the diabetes and pregnancy track I wanted to embark, but I have always been grateful that I found him and his open attitude to diabetes technology.
When CGM was launched into Australia, I spoke to my diabetes educator and asked her to fill in the required paperwork to get me sensing. She sent the form off the day we spoke.
And the same has happened when I have wanted to change or upgrade diabetes devices.
What I am trying to say is that this has all been led by me. So when A/Prof Varcoe spoke about the importance and value of connecting with PWD and telling them about these new vascular procedures to save limbs and prevent major amputations, it made perfect sense. He urged that we needed PWD to be the ones who, if told they needed to have an amputation, spoke up and asked for a second or third opinion, specifically asking about the very procedure he had just discussed.
This ground swell of action is what causes change, but we need to know exactly what to ask for. It’s far more effective to ask the question ‘Can my artery be revascularised? I understand there is surgery than can do that and may prevent the need for a major amputation.’ rather than just ‘Is there nothing more than can be done?’
So many of the people with diabetes I know are using particular drugs or devices because they have asked for them – not because they were recommended or suggested by their HCP. And this is why PWD need to have all the information. This is why device companies should be going straight to the consumer to share information, not expecting it to happen through HCPs. (I know that there has been discomfort from some HCPs at Abbott’s direct to consumer promotion of Libre – and the fact that PWD can order themselves without needing to see a HCP, but why would that be the case?)
But it is more than just making sure the information is there for PWD to know and see. It is a complete and utter reshaping of a system that a lot of times actually isn’t about empowerment. There are still too many ‘old school’, patriarchal attitudes that dictate care choices to the PWD instead of accepting and encouraging us to lead the way for our own care. I think things are changing, but I also think they are changing far too slowly.
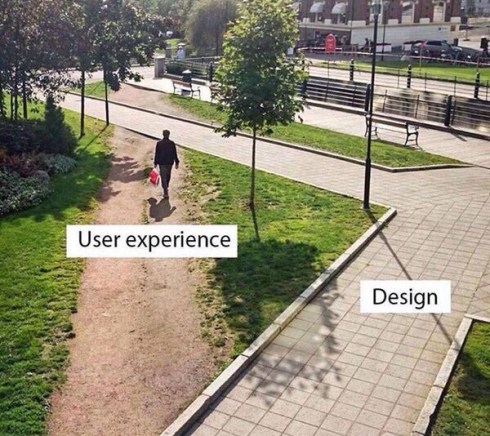
This photo* sums up why I do what I do, and why many people think I sound like a broken record, with a vocabulary of a mere seven words. Specifically, these seven words: ‘Have you spoken to people with diabetes?’
Because so often, the answer is ‘No’. Or ‘No – we’ll be doing that after we have had some meetings.‘ Or ‘Yes – we spoke to you‘ at which point I remind them that I pointed out when they did indeed speak to me that they should find other people with diabetes to speak with. Because I am but one person and speak for no one other than me. (Or, perhaps, another woman in her 40s who loves Nutella, boots, coffee, lives in inner-Melbourne, waves her hands around madly while speaking reallyreallyreallyreally fast, can recite Marx Bros movies from start to end, has what some would call an irrational fear of birds (and butterflies), can sing (badly) pretty much any song from the 1980s, has over 25 striped t-shirts in her cupboard and is battling an eleven year old daughter who has decided that she too loves stripes and wants to borrow all her mother’s clothes.)
Most people are not like that. (Fortunately.)
Anyway, this picture also demonstrates that those who have the privilege of designing services, activities, programs, settings for people with diabetes often miss the point – perhaps not by much, but nonetheless, they miss it. It’s usually because they forgot to ask us, or asked as too late, or didn’t keep coming back and asking and checking in. And then, when we don’t use what they design, we are branded ‘non-compliant’ or ‘disengaged‘ or ‘not interested in our health’, when the truth of the matter is that their design (without our input) just doesn’t fit our needs.
I have given so many talks and written so many pieces about this. But perhaps all I need is this on a t-shirt, tattooed to my arm (forehead?) and on the back of my business cards. Don’t design before speaking to the user. It’s actually really easy!
(*I don’t know the source of this photo, but if anyone does, please let me know so I can credit appropriately.)
So this happened….
Last night, I was the ‘here’s one we prepared earlier’ on a panel discussing CGM technology. The audience was all healthcare professionals – mostly DEs, but some dietitians, RNs and also a GP-in-training (so much yay to him for coming along!).
I love being in the room for these events! I wrote about my last experience giving the same talk here. I cannot speak highly enough of the two experts on the panel last night. Dr Peter Goss – who spoke at the last one of these events – is what I would call a disrupter in the diabetes healthcare space and, honestly, all the power to him. He may ruffle some feathers with his sometimes unorthodox approach, but it is undeniable that he is a champion for kids and teens (and young adults) with type 1 diabetes. Also on the panel was A/Professor David O’Neal who is best described as a truly awesome endo (I have heard that from every single person I know who sees him as their endo) and an absolutely brilliant mind. His expertise in diabetes tech is second to none and he is genuinely interested in how the technology can safely, efficiently and effectively be incorporated into the lives of people living with diabetes.
I know that all sounds rather effusive. But I need to point out that they are remarkable. And that they are the sorts of HCPs you want on your side if you are a person with diabetes.
Because now I am going to talk about language and why I pulled them up a little bit after we all did our presentations and sat on the stage ready to answer questions from the audience.
As happens frequently when I am in the room with a group of healthcare professionals, the conversation turned to language. Okay, I made that happen. In fact, the words I used were ‘I’m going to hijack this conversation because we really need to talk about language here.’
One of my biggest pet peeves is the jokey, and somewhat snide, comments made about people with diabetes making up numbers in their diabetes log books. Because, it’s not a joke. It’s not something for HCPs to roll their eyes over and dismiss as ‘non-compliant’ behaviour.
The word that was used for PWD who make up numbers in their books was ‘fakers’. I cringed the moment I heard the word. And cringed even more at the audience’s response – laughter, heads shaking from side to side and knowing looks. I looked around the room and knew that we would be talking about this later on in the evening!
As I pointed out when the panel was seated on the stage, I absolutely did this. And I was incredibly good at it – different coloured pens, splotches of blood on the pages, dog-eared corners of the book. Once, I even splattered a few drops of juice, because on that particular page, I was having a lot of lows and I thought the juice would make it look more authentic.
Now, let’s all just remember for a moment that I was diagnosed as an adult. This wasn’t insolent teenager behaviour. This was a woman in her mid-twenties who was terrified of disappointing and being judged by the HCP to whom she would be handing the grotty book and its made up numbers.
I told the room my story of this last night and there was laughter – because the way I spoke about it was amusing. It was a cheeky anecdote. But at the time, it wasn’t funny. I was scared, I hated checking my BGL, I was paralysed by numbers that didn’t make sense and I didn’t know what to do about it. So I lied. Of course my HCPs knew that. And I knew my HCP knew.
But the question is about WHY people do this. The discussion needs to stop being about diabetes at that point, because really, managing BGLs and most other diabetes tasks is not the issue here. The issue is distress, anxiety, fear. And, in my case, I felt desperate.
One of the panellists made the point that the reason that he brought it up was because HCPs need to know what to do when someone is ‘faking’ their numbers. He’s right. I completely agree. And then there needs to be understanding of how to approach it, which is likely to be different with each PWD.
For me, it took until I found a HCP who I felt I could trust – one who wouldn’t judge the numbers that were out of range (which one HCP always circled in red pen, making me feel even more like a delinquent adolescent) – and was interested in knowing what was stopping me from feeling able to check my BGL.
When we worked through that, I was better equipped to not only regularly check my BGL, but also to deal with the numbers and act upon them. I came to understand that a number was nothing more than a piece of information that I could use to make a treatment decision – not an indication of me being a good or bad person.
Language does matter. And words count for a lot. Using the word ‘faker’ in this context is loaded with judgement and accusation, and even if that is not the intention, it made me – a person with diabetes – feel very uncomfortable. But mostly, it fails to consider the real problem at hand which is not that a PWD is making up numbers in a book. It is why they feel the need to do that.




 It’s about words, because language matters and sticks with us forever.
It’s about words, because language matters and sticks with us forever.