You are currently browsing the category archive for the ‘Health’ category.
This is a transcript of a talk I gave earlier this year to a European-based health consultancy and creative agency about my take on global diabetes community-based advocacy – the opportunities and challenges. The title I was given was ‘Making Engagement the norm rather than the exception’. AI did a remarkably decent job with this transcript, but I expect that there might be some clunky language in there that I missed when I read through it on a plane after being in transit for 27 hours straight. Or, I could simply have used clunky language. Either way, it’s my fault.
I often say that community is everything, but I want to begin by saying that it’s important to understand that there is no single, homogenous diabetes community. Everyone’s diabetes experiences are different. I truly believe that there are some issues that unite us all, but really, we are a very disparate group – something I have come to understand more and more the longer I have been involved in diabetes community advocacy. This poses possibly the largest challenge for everyone in this room wanting to work with “THE diabetes community” because if you’re looking for a group that agrees on everything and believes the same thing, I’m sorry to say that you’re going to be in for quite a ride!
But it is also the biggest opportunity – and the way to get an edge – because it gives anyone who works in the diabetes space – from healthcare professionals, researchers, industry, diabetes organisations, policy makers, the media – to roll up their sleeves and make a concerted effort to talk with a wide range of people with diabetes to understand our experiences and what we need. Look, I know that it would be easier for all of you if I said, ‘Speak with one person and then you’re good to go’, but that would be a lie. Sadly, a lot of people and organisations still believe this to be the case, and I have a great example to show you why that doesn’t work.
And that example? It’s me, hi, I’m the problem, it’s me.
A number of years ago, a researcher reached out to me with an invitation to be the ‘consumer representative’ on their project. After bristling at the term “consumer”, I asked what the project was about, and this is what they said, word for word because I wrote it down and have told this story a million times as a cautionary tale: ‘It’s a project on erectile dysfunction in men with type 2 diabetes, diagnosed over the age of 65.’
There was not a note of irony in this invitation. When I pointed out that I fit literally none of the categories in the study and then went on to point out that I am a woman; I have T1D; no erectile dysfunction; diagnosed at 24; was not within a decade of 65 years of age, the response was ‘Oh, but you have diabetes, so you’ll be great’.
Friends, I would not have been great.
For the purposes of this discussion, when I say diabetes community, I am referring to people with lived experience of diabetes. There is a lot of cross over in the diabetes advocacy space, and there are many examples I can point to that show how valuable advocacy efforts can be when people with diabetes are involved in efforts led by diabetes organisations or other stakeholders. In fact, at the end of last year, we saw a brilliant example of that with Breakthrough T1D in Australia receiving $50.1 million in funding from the Australian government for their Clinical Research Network. This is the power of an organisation meaningfully engaging with their community to tell the story of why their advocacy is important. I mean, what is more compelling than hearing from people with diabetes and their families about how research holds the key to a better diabetes future?
I’d encourage you to look at Breakthrough T1D Australia’s socials to see just how beautifully they centred people with lived experience to get their message across, and how it was people with diabetes who literally marched on parliament to tell the story. The coordination of the campaign may have come from a passionate advocacy and comms team in an organisation, but the words were all people with diabetes. (For transparency: I work for Breakthrough T1D, formerly JDRF, but not for the Australian affiliate. I am, however, extraordinarily proud of what Breakthrough T1D Australia has achieved and so, so impressed with the way their communications campaigns are never about the organisation or staff, but rather about the community.)
I believe that our community excels in telling the stories of our lives with diabetes, what we need to make our lives better, what works in our communities and how we can better work together. Some standout examples of this include the #dedoc° community, and, in particular, the #dedoc° voices scholarship program. This is the only truly global community where diabetes advocates are not only present but are leading conversations. #dedoc° has no agenda other than to provide a platform for people with diabetes which results in diverse stories and experiences being heard. And it also means that organisations want to work with #dedoc° because it’s an easy way to connect with community. (And another point of transparency: I’m the Head of Advocacy for #dedoc°.)
Organisations that thrive on working with community demonstrate their commitment to improving the lives of people with diabetes in ways that matter. If you don’t know about the Sonia Nabeta Foundation (SNF), you really should! The foundation has a network of ‘warrior coordinators’ who provide peer support and a whole lot more! I have now had the honour of chairing sessions at international conferences with four of these warrior coordinators and I can say without a doubt that Hamida, Moses, Nathan and Ramadhan’s stories resonated and stayed with the audience way beyond the allotted ten minutes of their talks. Addressing the challenge of a limited workforce and resources by engaging and employing people with diabetes to educate and support younger people with diabetes is so sensible and clever. And the results are remarkable.
I have seen similar examples in India. Visiting Dr Archana Sarda’s Udaan centre in Aurangabad and Dr Krishnan Swaminathan’s centre in Coimbatore completely changed my understanding of peer-led education. And groups like the Diabesties Foundation and Blue Circle Diabetes Foundation (also in India) are prime examples of the successes we can expect when people with diabetes take charge of programs and lead diabetes education.
Seeing these examples firsthand lit a fire under me to challenge what we have been told in high-resourced countries like Australia, and here across high-income countries in Europe. Why is it that we, as people with diabetes, are told to stay in our lane and not provide education? We may be considered ‘higher resourced’, but people fall through cracks because they are not getting what they need. Health systems remain challenged and overwhelmed.
The challenge we have in places like Australia is that PWD are very clearly told that we are not qualified to provide education. Rubbish! Our lived experience expertise puts us in the prime position to do more than just tell our own story, and I believe we need to boldly push back on beliefs that only health professionals are equipped to fill education and knowledge gaps. Because in addition to what we know, the expertise we hold and our ability to speak in the language that PWD understand, we also know about ‘going to the people’ and not expecting a one size fits all approach to work.
It would be naïve to think that community-led, and -driven programs and initiatives aren’t already happening. Community is integral in providing information that PWD are desperate for, even with caveats about consulting HCPs. There are 24/7 support lines available in the community, something that is simply not available in most healthcare settings. And anyway, who better than others with diabetes to give practical advice on real life with diabetes than those walking similar paths? In the moment and with direct experience.
The #WeAreNotWaiting community was established to not just offer advice but develop technologies to improve lives of people with diabetes and continues to do so today. A five minute lurk in any of the online community groups dedicated to open-source technologies is all it takes to see people with diabetes who had been at the end of their tether with conventional care now thriving thanks to community intervention.
And that is replicated in low carb groups where community provides advice and education on how to eat in a way that is often not recommended by HCPs. People share experiences how they are flourishing thanks to making informed decisions to eat this way, and air their frustrations about how they are often derided by HCPs about those decisions. The support that comes from these groups is often just as focussed on how to deal with the healthcare environment when going against the grain (unintended pun) as sharing ideas and advice on how the science behind how low carb diets work.
T1D groups talk about incorporating adjunct therapies into their diabetes management, moving from a glucose-centric approaches to looking at other meds and interventions that can support better outcomes. GLP1s may not be approved for use by people with T1D, but they are increasingly being used off label because of their CVD and kidney protective nature. These community discussions include suggestions on how to have conversations with HCPs to ask about how adjunct therapies might help, including pushing back if there is a blanket ‘no, it’s off label’ response. Before anyone thinks this isn’t a good thing, I remind you that we still need prescriptions from our HCP before we can start on any new drug. We should be listened to when we ask to have a discussion about new and different ways to manage our diabetes.
And there are also businesses led by community that have stepped into spaces that are traditionally organisation or HCP-led. A few years ago, Aussie woman Ashley Hanger started Stripped Supply to fill a massive gap when diabetes supplies could no longer be ordered online and shipped, instead necessitating a backstep where PWD had to go into pharmacies to pick up supplies. Ashley’s start up gave the people what we wanted and meant that, for a small subscription fee, supplies could be straight to our doors again. And it’s run by community – what’s better than that?
There is contention about people with diabetes working with industry, and that is a conversation for another time. But I will say that when we have people with diabetes involved in the development of the devices that we use and/or wear on our bodies every day, the end products are better. That’s just a fact. When you have people with diabetes employed by device manufacturers writing education and instruction manuals for those devices, they make sense because they are written from the perspective of someone who actually understands the practical application of using those devices. It’s a massive opportunity for industry to engage – and employ – people with diabetes. Way to get an edge!
What I would say to everyone here today is that if you are not directly working with people with lived experience of diabetes, you are missing out on the biggest piece of the diabetes stakeholder puzzle. But you have to do it meaningfully and perhaps the biggest challenge I face is dealing with the rampant tokenism that exists in the diabetes ecosystem. For my entire advocacy career I have been urging the implementation of meaningful engagement, and to be honest, a lot of the time I feel that I have failed in those attempts. Every time I see a crappy program or campaign come out of somewhere that claims to work with community, I realise that people with diabetes are being used in possibly the most nefarious way possible: to ‘lived experience wash’ the work of the organisation. I wrote a piece earlier this year about this and was completely and utterly unsurprised to receive comments justifying poor attempts of consultation.
But then, I see something like the video I am going to finish with from Breakthrough T1D in the UK, and I know that there is intent there to do the right thing and do it properly. To involve people with diabetes from the beginning, and centre them throughout the work. The result is a beautiful piece of storytelling that has been shared across the globe. I don’t know the metrics, and quite frankly, I don’t care. All I need to see is the response from the community to know and understand that this hits the spot. And you can too with your work if you engage properly. We’re here to help.
You can watch What a Cure Feels Like, the Breakthrough T1D UK video that concluded my talk here.
Disclosure
I was invited by a health consultancy firm to give a talk to fifty people working on public-facing health campaigns (NDA, can’t say anything more) and then run a workshop about working with lived experience representatives. I was paid for my time to present and prepare for the session, and reimbursed for ground transfers to and from the location of the meeting.
Last week I was in Geneva for the 78th World Health Assembly (WHA78). It’s always interesting being at a health event that is not diabetes specific. It means that I get to learn from others working in the broader health space and see how common themes play out in different health conditions.
It’s also useful to see where there are synergies and opportunities to learn from the experiences of other health communities, and my particular focus is always on issues such as language and communications, lived experience and community-led advocacy.
What I was reminded of last week is that is that stigma is not siloed. It permeates across health conditions and is often fuelled by the same problematic assumptions and biases that I am very familiar with in the diabetes landscape.
I eagerly attended a breakfast session titled ‘Better adherence, better control, better health’ presented by the World Heart Federation and sponsored by Servier. I say eagerly, because I was keen to understand just how and why the term ‘adherence’ continues to be the dominant framing when talking about treatment uptake (and medication taking). And I wanted to understand just how this language was acceptable that this was being used so determinately in one health space when it is so unaccepted in others. This was a follow on from the event at the IDF Congress last month and built on the World Heart Foundation’s World Adherence Day.

While the diabetes #LanguageMatters movement is well established, it is by no means the only one pushing back on unhelpful terminology. There has been research into communication and language for a number of health conditions and published guidance statements for other conditions such as HIV, obesity, mental health, and reproductive health, all challenging language that places blame on individuals instead of acknowledging broader systemic barriers.
I want to say from the outset that I believe that the speakers on the panel genuinely care about improving outcomes for people. But words matter as does the meaning behind those words. And when those words are delivered through paternalistic language it sends very contradictory messages. The focus of the event was very much heart conditions, although there was a representative from the IDF on the panel (more about that later). But regardless the health condition, the messaging was stigmatising.
The barriers to people following treatment plans and taking medications as prescribed were clearly outlined by the speakers – and they are not insignificant. In fact, each speaker took time to highlight these barriers and emphasise how substantial they are. I’m wary to share any of the slides because honestly, the language is so problematic, but I am going to share this one because it shows that the speakers were very aware and transparent about the myriad reasons that someone may not be able to start, continue with or consistently follow a treatment plan.
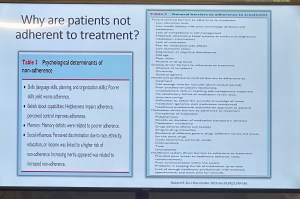
You’ll see that all the usual suspects are there: unaffordable pricing, patchy supply chains, unpleasant side effects, lack of culturally relevant options, varying levels of health literacy and limited engagement from healthcare professionals because working under conditions don’t allow the time they need.
And yet, despite the acknowledgement there is still an air of finger pointing and blaming that accompanies the messaging. This makes absolutely no sense to me. How is it possible to consider personal responsibility as a key reason for lack of engagement with treatment when the reasons are often way beyond the control of the individual?
The question should not be: Why are people not taking their medications? Especially as in so many situations medications are too expensive, not available, too complicated to manage, require unreasonable or inflexible time to take the meds, or come with side effects that significant impact quality of life. Being told to ‘push through’ those side effects without support or alternatives isn’t a solution. It is dismissive and is not in any way person-centred care.
The questions that should be asked are: How do we make meds more affordable, easier to take, and accessible? What are the opportunities to co-design treatment and medication plans with the people who are going to be following them? How do we remove the systemic barriers that make following these plans out of reach?
One of the slides presented showed the percentage people with different chronic conditions not following treatment. Have a look:

My initial thought was not ‘Look at those naughty people not doing what they’re told’. It was this: if 90% of people with a specific condition are not following the prescribed treatment plan, I would suggest – in fact, I did suggest when I took the microphone – the problem is not with the people.
It is with the treatment. Of course it is with the treatment.
The problem with the language of adherence is that it frames outcomes through the lens of personal responsibility. It absolves policy makers of any duty to act and address the structural, economic and systemic barriers that prevent people from accessing and maintaining treatment. Why would they intervene and develop policy if the issue is seen as people being lazy or not committing to their health?
And it means the healthcare professionals are let off the hook. It assumes they are the holders of all knowledge, the giver of treatment and medications, and the person in front of them is there do what they are told.
There is no room in that model for questions, preferences, or complexity. There is no room for lived experience. There are no opportunities for co-design, meaningful engagement or developing plans that are likely to result in better outcomes.
When the room was opened up to questions, I raised these concerns, and the response from the emcee was somewhat dismissive. In fact, she tried to shut me down before I had a chance to make my (short) comment and ask a question. I’ve been in this game long enough to know when to push through, so I did. I also don’t take kindly to anyone shutting down someone with lived experience, especially in a session where our perspective was seriously lacking. Her response was to suggest that diabetes is different. I suggest (actually, I know) she is wrong.
And I will also add: while there was a person with lived experience on the panel, they were given two questions and had minimal space to contribute beyond that. I understand that there were delays that meant they arrived just in time for their session, but they were not included in the list of speakers on the flyer for the event while all the health professionals and those with organisation affiliation were. There comments were at the very end of the session, and I was reminded of this piece I wrote back in 2016 where health blogger and activist Britt Johnson was expected to feel grateful that the emcee, who had ignored her throughout a panel discussion, gave her the last five minutes to contribute.
Collectively this all points to a bigger issue, and we should name that for what it is: tokenism.
I didn’t point this out at the time, but here is a free tip for all health event organisers: getting someone to emcee who is a journalist or on-air reporter does not necessarily a good emcee make. Because when you have someone with a superficial understanding of the nuance and complexity involved in living with a chronic health condition, or understand the power dynamics and sensitivities required when facilitating a conversation about long-term health conditions, you wind up with a presenter who may be able to introduce speakers, but you miss out on meaningful and empathetic framing of the situation. There are people with lived experience who are excellent emcees and moderators, and bring that authenticity to the role. Use them. (Or get someone like Femi Oke who moderated the Helmsley + Access to Medicine Foundation session later in the day. She had obviously done her homework and was absolutely brilliant.)
I know that there has been a lot of attention to language in the diabetes space. But we are not alone. In fact, so much of my understanding has come from the work done by those in the HIV/AIDS community who led the way for language reform. There are also language movements in cancer care, obesity, mental health and more. And even if there are not official guidelines, it takes nothing to listen to community voices to understand how words and communication impact us.
So where to from here? In my comment to the panel, I urged the World Heart Foundation to reconsider the name of their campaign. Rather than framing their activities around adherence, I encouraged them to look for ways to support engagement and work with communities to find a balance in their communications. I asked that they continue to focus on naming the barriers that were outlined in the presentations, and shift from ‘How to we get people to follow?’ to ‘How do we work with people to understand what it is that they can and want to follow?’.
Finally, it was great to see International Diabetes Federation VP Jackie Malouf on the program on the panel. She was there to represent the IDF, but also brought loved experience as the mother of a child with diabetes. The IDF had endorsed World Adherence Day and perhaps had seen some of the public backlash about the campaign and the IDF’s support. Jackie eloquently made the point about how the use of the word was problematic and reinforced stigma and exclusion, and that there needs to be better engagement with the community before continuing with the initiative.
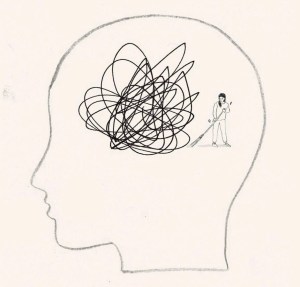
I’ve been unwell.
And so, I’ve had time to think. Mind you, I’ve found it difficult to form thoughts properly, thanks to the brain fog that is impacting my attention span and ability to think things through to a conclus…oh look! The leaves on the trees in the garden are changing. I should buy the last plums when I go to the fruit and veg shop, and bake a plum cake. That would be delici… Are mandarins in season yet? Ooh, a puppy!
Anyway, back to trying to focus on what I’ve been randomly and messily thinking about.
On my last day at ATTD in Amsterdam, I wound up with a very weird pain flare that meant I could barely move. I put two and two together, came up with the wrong answer and decided it was thanks to arthritis and spent the day before my flight desperately trying to sleep it off so I would be okay to navigate Schiphol Airport and get myself home. I did make it home, but not without wheelchair assistance at each airport, and in excruciating pain for the entire long trip home.
Turns out, it wasn’t arthritis. It also wasn’t diabetes, but that didn’t stop me from trying to connect non-existent dots.
The day before the paralysing pain flare, I woke at 3am with my Dex alarm wailing. I was low. Very low. For five hours. You know, one of those lows that just won’t quit. One of those lows that simply won’t respond to massive quantities of glucose. I ended up throwing up after force feeding myself jellybeans and guzzling juice from the minibar, which was all just lovely. (And yes – I realised I had some inhalable glucagon with me AFTER the fact … but in my low fog, forgot as I was just trying to stay alive with sugar.)
Of course, I was exhausted when I finally came back in range and felt like I’d been hit by a truck. But sure enough, I got up and had a frantic day at the conference centre, in meetings, giving talks and trying to appear functional while feeling absolutely wrecked.
The next day, when I woke up unable to move because I was in pain, I thought that perhaps it was a result of overdoing things the day before, when I should have perhaps taken the morning off to recover from the hypo and the exhaustion that came with it. But of course I didn’t. Because when have I ever taken time off for diabetes? One time I had an evening black out hypo in a park requiring paramedic attention and I was in at work at my desk by 8.30am the next day. Because why wouldn’t I be? My weird and illogical attitude is that if I was to take time off to recover every time diabetes doesn’t play nicely, I’d be taking hours off each week. No one has time for that. At least, I certainly don’t.
And how very messed up that thinking is. I realise that. And I know what I say to friends with diabetes who tell me about their particularly crappy hypos, or when diabetes is kicking their arse/ass: ‘Take the time and let your body rest,’ I’ll say. ‘You’ve just been dealt a pretty shitty blow to your body and mind. Don’t overdo it,’ I’ll remind them.
And what do they do? They don’t rest. They don’t listen to their body. They overdo it. It’s what we do.
It’s messed up and we keep doing it, even though we know better. Of course we know better: because we give good advice to others. But we then do that ridiculous thing where we think resilience is strength, where actually, resilience would be listening to what our bodies need and then doing it. We ignore symptoms and give ourselves imaginary gold stars for ‘pushing through’.
It took some weird virus that literally hampered my ability to walk for me to take time off work. Sleeping 20 hours a day was all I could manage. But you know what? I should have slept 20 hours the day after the five-hour low to recover too, but of course I didn’t.
Who am I trying to impress by soldiering on as though there’s nothing wrong? What am I trying to prove? Do I think we get extra points in some bizarre Hunger Games-like challenge? Is it that I worry what others will think of me if I say, ‘I need to stop for a bit’? Am I afraid of seeming weak? Lazy? Or am I – twenty-seven years later – trying to live up to the ‘diabetes doesn’t change anything’ line I was fed the day I was diagnosed, even though it changes everything?
I’ve been back home now for two weeks now and really just getting back to regular programming now. On Sunday I was able to stand up for long enough to bake a cake. That was a win. I also was able to walk to our local café – a five-minute walk away – but needed a lift home. Slowly, but definitely better.
I’m not pushing myself – partly because I can’t, but also because I refuse to and that is something that is very weird for me. I’m home this week instead of flying to Bangkok to speak at the IDF Congress – the first time I have ever cancelled a work trip. Usually I push through. Usually I suck it up and pretend all is fine. Because I drank the ‘diabetes-won’t-stop-me’ Kool Aid when instead, I should have recognised that there is no shame in stopping to rest. I need to be better and do better about this. And listen to the advice I would give everyone else. Permission to take time out for diabetes.
This post is dedicated to my darling friend and #dedoc° colleague Jean who also doesn’t know when to stop. Let this be a reminder to put down the Kool Aid!

Is it too late to say Happy New Year? Probably, but does anyone actually believe that social norms still exist in the world the way it is these days?
And so – happy New Year to you. I’ve been absent. Not that it’s important to acknowledge this. But I have been because headspace these days is non-existent because of (gesturing wildly) the world.
But anyway, here’s an update no one asked for, (actually not true – thanks to all the people who have reached out and asked):
I made a resolution. Happy to hear that many of you have made a similar one. Smart, smart people!
I also didn’t do things: I didn’t start some bullshit diet, because diet culture sucks and is harmful. I didn’t tell anyone what they should be eating, because no one needs that. I didn’t go away for the holidays, because I was so travel burned out that the last thing I wanted to do was jump on an aeroplane.
Instead, I read some great books (Amor Towles, Jhumpa Lahiri, Paul Auster’s final words) and read some not-so-great books (Stanley Tucci – I adore you, but your latest book could have stayed as a personal diary and not been published, mate). Walked lots. Sat outside in cafes drinking barrel-loads of iced coffee. Saw some movies and binge-watched some TV shows (do we need to talk about Apple Cider Vinegar? Yes, yes we do.)
And I spent a lot of time complaining about my hands. My sore, achy, stiff, stupid hands.
I now have arthritis. Is it because I am old? Or maybe just because I collect health conditions? Is it psoriatic arthritis or is it osteoarthritis? (Probably both.) Does it have anything to do with perimenopause? Is Mercury in retrograde? Did I walk under a ladder? Whatever the reason, it sucks. And it hurts.
This diagnosis actually came last year, so I don’t really get to blame 2025 for it. It started in September. One day, I didn’t have pain in my fingers. And then I did. I spent the whole time I was in NY for the UNGA last year noticing that a lot of the time I moved my index fingers I felt a little twinge. Then the twinge moved to other fingers. By the time I was on the plane home there was pain any time I moved my hands. And even when I didn’t. So pretty much all the time.
These are the hands that type words, make divine cakes and pastries, roll out pasta dough, turn the pages of books, hold onto my loved ones, grasp microphones on conference stages and in media opportunities, press down on cutters as I shape biscuit dough, hold the cups containing the coffee that sees me through the day, doom-scroll through the latest update in the cesspit of the world, tickle the tummies of our dogs, pat the top of the head of our cat, point out the specific pasticcino at the pasticceria I want to eat, stir pots of delicious soups and sugo on the stovetop, tap out snappy responses to misogynists on the internet, are waved around as I talk… And all of these things cause pain. All of them.
Here’s something about me: I don’t deal well with pain. I had a little cry in my GP’s office at the end of last year. I cried because there isn’t something I can do to just fix this. Here’s the list of things I read that I should do to help improve arthritis pain: be a ‘healthy’ weight (because diet culture and we’re led to (falsely) believe that people who live in smaller bodies are always perfectly well. Bullshit), stop smoking, limit alcohol, eat healthily, walk and be active. I can’t start to do those things because I already tick each and every box. So what I am supposed to do? Sure, my activity involves little more than walking, but I do get in close to if not 10,000 steps a day, so I’m not completely sedentary.
I’m whingy about it all because the pain is always there, and I don’t get a break. And diabetes is always there, and I don’t get a break. And anxiety is always there, and I don’t get a break. Honestly, I’d take the pain not being there and keep the others any day.
While I wait to see a rheumatologist, I am doing some things that may be easing the pain a little. I say ‘may’ because I don’t really know, and I don’t want to stop them in case it makes it worse. And I spend a lot of time annoying people by telling them my hands hurt. (Don’t believe me – see the 800 words in this blog post – thanks for reading!)
I know the world doesn’t work this way, but sometimes I think it would be nice if those of us already dealing with a shedload of health conditions could sit things out for a bit. By ‘things’ I mean new diagnoses. That would be fair, wouldn’t it? I don’t really want to add another health professional to my contacts list and dedicate more time in my calendar for regular check-ups. And I don’t want to have to learn the lingo of a new health condition, while training a new HCP to understand the way I like to be treated. I don’t really want to have to give more money to the pharmacist for more drugs. I don’t really want to use more emotional bandwidth worrying and thinking about what this means long term. I don’t want to think about being in pain all the time. I also don’t want to wind up not being able to wear the beautiful rings I own, and feel free to call me shallow while I completely ignore you.
And so, that’s where I am right here and now. A mostly gentle start to the year. And sore hands. Very, very sore hands.
When the clock ticked over into 2025, I had no intention of even considering coming up with New Year’s resolutions that would shape my new year. But with all that is going on in the world, I’ve given myself permission to reconsider and do all I can to stick to it. And I’m encouraging everyone I know to make the same resolution.
And that resolution is to do a health literacy check-up and to actively pushback against misinformation. There has never been a time when being health literate is more important. I thought that during the COVID years as we received a daily onslaught of misinformation about vaccines, bogus treatments (bleach, anyone?), outright lies (“it’s just a cold”) and conspiracy theories (“BigVax is behind it all”). But how naïve I was. Those days seems like just a warm-up for what is happening today.
I’m in Australia, but I don’t for one moment think we are immune to the madness sweeping the world. But if you are shaking your head and laughing a little when RFK Jr spews his anti-vax, anti-fluoride, anti-science agenda, or Dr Oz uses his latest pseudoscience claim as the foundation for whatever supplement he is selling, you’re not grasping the seriousness of what is going on. Before we Aussies get too smug, we should remember our own backyard isn’t devoid of charlatans, and it’s only a matter of time before someone like Pete Evans is taken seriously in public health discussions. Think I’m over-reacting? He already made a run for the senate. How long before a conservative party sweeps him into their fold?
I think it’s safe to say that we have moved beyond this sort of misinformation being a fringe issue amongst ‘crunchy’ parents, trad wives and ‘wellness’ influencers. And Gwyneth Paltrow.
Health misinformation is deliberate and it’s mainstream, and protecting yourself against it isn’t optional – it’s essential.
Up until now there have been guardrails in place to protect public health. Boards and regulatory agencies have existed to ensure medical safety and provide us with confidence that there are processes in place to determine the safety of drugs, devices, healthcare programs. Guidelines are based on robust and rigorous research and are developed using evidence and expert consensus. (Side bar: Have people with lived experience been involved in these practises? Absolutely not enough. Could this be better? Absolutely yes.)
Critical thinkers understand that science is not static. We understand that science changes as evidence evolves. We also understand that we don’t have to follow guidelines blindly. We should understand and consider them. And then use them to make informed health choices. I repeatedly say this to anyone who questions off label healthcare (my favourite kind of healthcare!): ‘I understand guidelines and learn the rules so I can break them safely’. That’s what being health literate does – it gives me an understanding of risks and benefits to make decisions about my health and what works best for me. And it gives me confidence to spot and push back on misinformation.
Critical thinkers also know that questioning medical advice is not the same as embracing conspiracy theories. It doesn’t mean throwing the baby out with the bathwater as you hastily reject modern medicine in favour of snake oil salespeople. It certainly doesn’t mean denying the effectiveness of a vaccines. And it doesn’t mean trusting Instagram wellness influencers.
More than ever, now is the time to do some questioning – to question who is spreading health information and consider their motives. What are they selling? (Case in point: Jessie Inchauspe who offensively calls herself ‘Glucose Goddess’ while selling her ridiculous ‘Anti Spike’ rubbish as she spreads fear about perfectly normal glucose fluctuations in people without diabetes). And a question that right now should be front of everyone’s mind: What power grab is behind the way someone is positioning themselves as an oracle of health information?
This post is about health literacy in general, but because this blog is called ‘Diabetogenic’ and I have diabetes, most people reading will be directly impacted by diabetes. And if there is any silver lining in this shitshow, it’s this: We’ve been dealing with health misinformation about our condition for decades, so in some ways, we’re probably ahead of the curve. We’ve had to wade through the myriad cures and magic therapies, the serums and pseudo-therapies. And the cinnamon – so much cinnamon! We’ve been standing up for science, challenging misinformation, and ensuring that diabetes health therapies are based on evidence, not fairytales. We’ve expected truth in our healthcare. It’s seemed the normal thing to do. Now it feels like a radical act to be a critical thinker.
We are a crucial point because health is being weaponised more than ever. Someone told me the other day that my lane is diabetes and health, and I should leave politics out of it. It’s laughable (and terrifying) to think that anyone doesn’t understand that health is political. It always has been. And even more so right now. We are seeing in real time political figures (and rich white men who own electric car companies) weaponise health misinformation for their own agendas, and scarily people are listening to them. They are elevating unqualified voices and aligning with conspiracy theorists, giving dangerous misinformation legitimacy. (And if you think that it’s all eerily familiar, you’re right. It’s already happened with climate change.)
Your radical act is to be smarter, to be more critical, to question sources and motives; follow reputable sources, don’t share viral posts before fact checking (Snopes is super useful here). Don’t reject credible advice and information in favour of conspiracy theories. Stack your bookshelves with books by qualified experts (I’d recommend starting with Jen Gunter’s holy trinity – The Vagina Bible, The Menopause Manifest and Blood and Emma Becket’s You Are More Than What You Eat), including lived experience experts who base their healthcare on legitimate evidence. Follow diabetes organisations like Breakthrough T1D (JDRF in Australia) for research updates and community efforts and be smart about which community-based groups you join. If moderators are not calling out health misinformation, I’d be questioning just how the group is contributing to diabetes wellbeing.
We know knowledge is power. But that knowledge base has to be grounded in fact, not fiction. Health literacy is critical because misinformation isn’t going anywhere, and neither are the people pushing it for profit and power. My resolution is to sharpen my critical thinking skills, ask questions, and refuse to let bad science set us backwards and cast a dark shadow over the health landscape. Who knew something so fundamental could be such a radical act?

Colour me unsurprised they couldn’t back up their claim with evidence.
The TGA has, once again, advised that Ozempic shortages in Australia are ongoing and in their brief statement they say this:
Sounds easy enough and it would be if only the issue of Ozempic prescribing was black and white and supremely simple which, sadly, it isn’t. There is confusion and frustration as people using Ozempic – both who do and don’t meet the criteria – find it difficult to maintain supply. People who don’t meet the criteria are sometimes being shamed for trying to access it and told that they are not deserving.
Firstly, let’s get the disclaimers out of the way: I am not a healthcare professional. I am not providing medical advice. I am not endorsing any sort of therapy or treatment (on- or off-label.) I am a person with T1D who is inherently interested in access to technologies and medicines that make our lives better. And I am interested (and believe) in off-label use of technologies and drugs because my diabetes life and overall health have been greatly improved by using different therapies off label. Also, in case you need a reminder, pretty much all people with diabetes behave off label in some ways, and if you don’t believe me, just ask someone with diabetes when they last changed their lancet.
And a little reminder that I don’t work for any Australian-based diabetes organisations, so this is not in any way aligned, or affiliated with what organisations are saying, or not saying. This is me, an Aussie punter with T1D, sharing my thoughts. (As I have done in the 2,000 plus posts on here already.)
Okay, with that out of the way, here are my thoughts – and my frustrations – with the latest on the Ozempic shortage saga.
In Australia (and in other places, but I live here and therefore am confined by Australian prescribing rules), the TGA has indicated Ozempic is use for the following (and excuse the language – the TGA needs me to come back and give them a little #LanguageMatters update):
‘the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise:
- as monotherapy when metformin is not tolerated or contraindicated.
- in addition to other medicinal products for the treatment of type 2 diabetes.’
For people who meet these criteria, Ozempic is prescribed using a PBS prescription which means that the cost will be $31.60 (or $7.30 for concession card holders) for one pen.
Does this mean that ONLY this cohort can have Ozempic prescribed for them? No, no it does not. Off label prescribing is not all that uncommon (not just for Ozempic, I’ll add). For people who do not meet the eligibility criteria, Ozempic is prescribed using a private prescription and the cost will be around $140 for one pen.
Is Ozempic being prescribed off-label? Of course it is. Increasingly so.
Anecdotally, I hear from many, many friends with T1D in Australia, but especially in the US, who are also using Ozempic in their diabetes management arsenal. I have heard dozens of talks at conferences in the last couple of years where T1D management is moving further and further from being gluco-centric with an approach that looks at drug combinations that address insulin resistance, lipids, blood pressure, heart and kidney health. It makes sense. As people in higher income countries have access to highly sophisticated hybrid-closed loop systems which significantly increase our TIR, and have us easily reaching HbA1c targets, many of us are looking to see what adjunctive therapies can support our broader health. GLP-1s are shown to have CVD and kidney protective benefits – something that many people with T1D are keen to access. In a talk at the Australian Diabetes Congress this year, head of EASD, Professor Chantal Mathieu said: “These medications are organ-protecting agents”.
The TGA announcement fails to recognise in any way that Ozempic is being used for other purposes than weight loss, and that it can be beneficial to people with T1D.
But let’s look beyond my own T1D bias for just a moment. There are many people with T2D who don’t meet the criteria set out by the TGA, yet who benefit greatly from Ozempic. Not only have they been denied accessing the drug at the PBS price but are also being denied supply completely for not meeting the criteria. Yet, many fear if they stop using Ozempic, they will find themselves meeting the criteria because their glucose levels will go out of range. This cohort feels like they are in complete and utter limbo and not being supported to use the medication that is drastically improving their glucose numbers and their overall health. A quick look in any online diabetes group will see conversations about this – because they are happening every day.
And if we step out of the diabetes sphere, people living with obesity who have been told time and time again to lose weight to improve their health have found Ozempic to be hugely successful in addressing one of the modifiable risk factors of T2D. This is a prime example of damned if they do, damned if they don’t. This cohort is told to lose weight, but then the tools which support that are snatched away from them, and they are rapped over the knuckles for trying to access them.
I understand that there are shortages and with that, there will be priority groups. But completely ignoring that there are other groups who are benefitting from Ozempic and not even acknowledging them seems odd. As does ignoring the difficulties – including stigma, shame and judgement – that these groups are facing when it comes to trying to access medication that has been prescribed by their healthcare professionals. In fact, some might suggest it shows a glaring lack of understanding of community needs and experiences.
Postscript
I am aware that Wegovy is available in Australia and can be used by people for whom Ozempic is not indicated. Wegovy costs are at least double than Ozempic which means that it will be out of reach for people who are already being expected to pay private prescription prices for Ozempic.
It’s also perhaps worth mentioning that the use and endorsement of adjunctive therapies – including GLP-1s – in T1D is not new and is detailed in the Consensus report by the ADA and EASD about the management of adults with T1D. As is often the case, regulatory bodies are taking their time in catching up to medical consensus.
Stress impacts diabetes in different ways. And of course, everyone’s response is going to be different.
Before Loop (which now feels like almost a lifetime ago), the effect of stress on my glucose levels was tricky and unpredictable. At times, it would make me high. Other times, I’d be in Hypotown (the town no one wants to visit) for hours, without any respite. The clever Loop algorithm tidies most of that up for me these days.
But when it comes to diabetes, stress doesn’t only impact what I see on my CGM trace. It’s far more than that. Loop can only do so much… Insulin automation doesn’t mean diabetes automation. And it certainly doesn’t mean life automation.
Let me talk about how it’s affected things in the last couple of months …
To some, it might look as though I have become lazy about my diabetes management. I have run out of insulin in my pump more times than I care to admit, scrambling to find my spares bag to refill the canula. I ignore the alerts, silencing alarms and putting the task that needs to be done out of mind.
I’ve let the batteries on my pump and RileyLink wear almost right down. In fact, the batteries have got to the point where they are so crucially low Loop has stopped working. Even the Red Loop Of Doom on my Loop app hasn’t been enough to swing me into action.
I’ve almost run out of insulin. I never do this. Ever. I have a system that works for ordering new scripts to make sure that there is always at least two weeks’ supply, and then back up plans for my back up plans. And yet, there I was, staring down the last few drops of insulin in a penfill. I don’t use insulin pens. I use vials. But I’d run out of vials and was using a penfill that I have for absolute emergencies.
This had become an emergency.
Same goes for pump consumables. I was reduced to searching the depths of my diabetes cupboard and discarded handbags looking for an infusion set, desperately hoping that there was at least one, somewhere, that would do the trick before I had to knock on the door of my neighbour, asking her to tide me over.
This is one part of diabetes burnout for me – the way that I deal with my diabetes tasks. It’s not feelings of resentment that I must do those tasks; it’s not feeling distressed that I must do them. It’s not even feeling a paralysis about doing them. It’s simply not caring enough about them to take the time and energy to engage my brain and actually do it.
I know that when I am stressed, something’s gotta give, and for me, that’s always been doing diabetes.
I cannot tell you how much having automated insulin delivery sweeps up a lot of it. Forgotten boluses get sorted by Loop. Sure, it may take a little extra time and mean a bit of extra time above my upper range limit, but if I don’t engage, Loop will bring me back in range soon enough.
The low-grade nausea I’ve been living with for the last month means that eating is sometimes difficult, but I don’t even need to think about what that means for glucose levels, because Loop mostly does it for me.
And sleep! Sleep the gift that Loop keeps giving has been interrupted, not by diabetes, but by waking stressed. Or, as has happened twice in the last week, with a splitting headache, so painful that the throbbing has woken me from a deep sleep. Pre-Loop, sleep disturbances would wreak havoc with my glucose levels (often because most of the time those disturbances were because of my glucose levels). But now, as I see the upward spike start because I’ve been woken in the middle of the night and glucose is being dumped because apparently, I’m now up and awake, Loop kicks in with an ‘I don’t think so’, and that spike is shut down quickly.
But the nausea is debilitating physically. And being woken in the middle of the night is exhausting. And the stress is leaving me feel a little hopeless all around, to be honest. Teary, emotional, tired. And burnt out.
Many years ago, after a couple of periods of intense burnout, I did a smart thing and found a psychologist to help me. Together, we learnt to identify the triggers that precipitated burnout. This has truly become one of the most powerful tools in my diabetes emotional wellbeing arsenal, because learning when I am heading down the slippery slope of burnout, and realising it’s coming, has meant that I’ve been able to address it before I get so deep into that dark space, it becomes challenging to come back from.
So, right now, I know this is happening. I can feel the stress and the physical manifestation of it, and I can see how it is influencing my diabetes. Today, I spoke with my psychologist – in a way waving a white flag of surrender knowing that I need someone else to come in and help me through this, because I can’t do it myself.
The win is that I’ve seen it and I’ve recognised it. The win is I’m seeking help. The win is that I’ve caught it before I’m plunging to dark depths (I hope).
It’s not a win that I’m feeling this way. It’s not a win that this level of stress has started to affect so much, including my diabetes. It’s definitely not a win that I’ve reached the point where I’m staring down the path to diabetes burnout despite the reason being un-diabetes-related stress.
But that’s how it goes. Diabetes becomes part of it. Of course it does. Because diabetes is always part of it. Always part of everything. Always hand in hand with whatever else is going on. Stress and diabetes leading to burnout. One of the few equations in diabetes that I can count on.