You are currently browsing the category archive for the ‘Conferences’ category.
ISPAD has led the way when it comes to including people with lived experience of diabetes at their annual meeting. It was the first conference to work with #dedoc° to have a voices scholarship program. The society has included people with diabetes on the organising committee for some time. ISPAD has awarded the ‘Hero Award’ which recognises the work done by people in the community. And the conference scientific program involves people with diabetes speaking and chairing sessions.
And so, it was interesting to hear someone ask at last week’s meeting in Montreal whether there should be a limit to the involvement and number of people with diabetes.
I wasn’t actually in that session, but I certainly heard about it from many others. People seem to expect me to have words to say about these sorts of questions. Turns out I do – and so do other people. And there was quite a bit of discussion – both at the conference, and in an online group after I shared the question with members.
While the question may have been well intended, (I certainly don’t believe there was any malice in asking), it did make me bristle. The idea of limiting access to a diabetes conference to people with diabetes has never sat well with me. It reeks of gatekeeping. And it also sends the message that people with diabetes are ‘allowed’ at the discretion of others rather than having a right to attend.
I think that quantifying the number of any sort of participant is problematic, but I have always liked this pie chart drawn and tweeted by James Turner (@jamesturnereux, although he appears to no longer be on the cesspit site) from a Medicine X conference in 2017. I am pretty sure that I have already shared this somewhere in the #diabetogenic archives, because I think it’s great! What I like about this is that it recognises that everyone has an equal place to be there. That equilibrium does sit well with me!

I also like the comment from my friend, and researcher and fabulous diabetes advocate, Ashley Ng. We caught up today to discuss this issue, and she said ‘I don’t agree with a maximum, but I do think we need minimum representation by people with lived experience’.
But this isn’t just a matter of representation, and it’s not simple either. There is the broader issue of people with diabetes wearing more than one hat. Some may also be researchers, clinicians, involved in technology development, industry representatives and more. This certainly does point to the complexity of the ecosystem. When looking at the number of people with lived experience of diabetes, we draw the cohort from many different spaces.
But this in itself adds to the intricacies of the situation. In fact, it is something that I have spoken and written about for decades (most recently here) and my position is very clear, albeit not especially popular with everyone. I believe that people with lived experience who wear no other hat in the healthcare space must be prioritised for positions centring lived experience at conferences, in panels, on advisory groups and anywhere people with diabetes are intended to be represented. Why? Because these are usually the ONLY way for us to get a seat at the table. Those wearing other hats may find themselves able to access other pathways via their employment or professional settings.
This is why #dedoc° generally doesn’t offer scholarships to healthcare professionals and researchers. The voices program is for people with diabetes who otherwise would not be able to find a way to attend conferences and who don’t have other prospective funding opportunities. I am aware that HCPs and researchers have limited opportunities available to them, but there are funding streams and grants, and institutional supports that are simply not open to people with lived experience who do not have any professional affiliation. Of course, (and it shouldn’t need to be said, but I’ll say it anyway), I’m not minimising the experiences of those who bring both professional and personal perspectives. But there are so very few opportunities for people with diabetes who represent as community members only to find a seat at the table. Those seats should not only be reserved for us, but we should all work to protect them.
It would be remiss of me to not point out that there are indeed unique challenges for people who straddle the professional and lived-experience divide. This article (I am a co-author) was written by people with lived experience of diabetes and wearers of other hats and addresses some of the issues faced by people in this situation.
These discussions are always interesting, but they can be uncomfortable. And also frustrating. I would hope that we are far along the lived experience inclusion road to not have to justify the rights of people with diabetes to be part of conferences and other efforts. And rather than even suggesting gatekeeping, we should be looking at more ways to make access to these spaces easier, and focused on diversity of voices. Chelcie Rice says we should bring our own chair if there isn’t one already for us. I say, bring two or three and the people to fill them too. But honestly, we should be beyond that now, right? We should simply be able to walk into any space and take a seat.
Disclosure
ISPAD invited me to speak at this year’s meeting and covered by accommodation costs. Travel was part of my role at Breakthrough T1D.
Last week I was in Geneva for the 78th World Health Assembly (WHA78). It’s always interesting being at a health event that is not diabetes specific. It means that I get to learn from others working in the broader health space and see how common themes play out in different health conditions.
It’s also useful to see where there are synergies and opportunities to learn from the experiences of other health communities, and my particular focus is always on issues such as language and communications, lived experience and community-led advocacy.
What I was reminded of last week is that is that stigma is not siloed. It permeates across health conditions and is often fuelled by the same problematic assumptions and biases that I am very familiar with in the diabetes landscape.
I eagerly attended a breakfast session titled ‘Better adherence, better control, better health’ presented by the World Heart Federation and sponsored by Servier. I say eagerly, because I was keen to understand just how and why the term ‘adherence’ continues to be the dominant framing when talking about treatment uptake (and medication taking). And I wanted to understand just how this language was acceptable that this was being used so determinately in one health space when it is so unaccepted in others. This was a follow on from the event at the IDF Congress last month and built on the World Heart Foundation’s World Adherence Day.

While the diabetes #LanguageMatters movement is well established, it is by no means the only one pushing back on unhelpful terminology. There has been research into communication and language for a number of health conditions and published guidance statements for other conditions such as HIV, obesity, mental health, and reproductive health, all challenging language that places blame on individuals instead of acknowledging broader systemic barriers.
I want to say from the outset that I believe that the speakers on the panel genuinely care about improving outcomes for people. But words matter as does the meaning behind those words. And when those words are delivered through paternalistic language it sends very contradictory messages. The focus of the event was very much heart conditions, although there was a representative from the IDF on the panel (more about that later). But regardless the health condition, the messaging was stigmatising.
The barriers to people following treatment plans and taking medications as prescribed were clearly outlined by the speakers – and they are not insignificant. In fact, each speaker took time to highlight these barriers and emphasise how substantial they are. I’m wary to share any of the slides because honestly, the language is so problematic, but I am going to share this one because it shows that the speakers were very aware and transparent about the myriad reasons that someone may not be able to start, continue with or consistently follow a treatment plan.
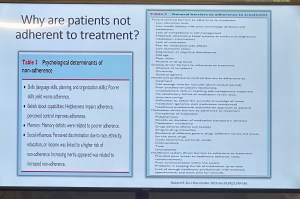
You’ll see that all the usual suspects are there: unaffordable pricing, patchy supply chains, unpleasant side effects, lack of culturally relevant options, varying levels of health literacy and limited engagement from healthcare professionals because working under conditions don’t allow the time they need.
And yet, despite the acknowledgement there is still an air of finger pointing and blaming that accompanies the messaging. This makes absolutely no sense to me. How is it possible to consider personal responsibility as a key reason for lack of engagement with treatment when the reasons are often way beyond the control of the individual?
The question should not be: Why are people not taking their medications? Especially as in so many situations medications are too expensive, not available, too complicated to manage, require unreasonable or inflexible time to take the meds, or come with side effects that significant impact quality of life. Being told to ‘push through’ those side effects without support or alternatives isn’t a solution. It is dismissive and is not in any way person-centred care.
The questions that should be asked are: How do we make meds more affordable, easier to take, and accessible? What are the opportunities to co-design treatment and medication plans with the people who are going to be following them? How do we remove the systemic barriers that make following these plans out of reach?
One of the slides presented showed the percentage people with different chronic conditions not following treatment. Have a look:

My initial thought was not ‘Look at those naughty people not doing what they’re told’. It was this: if 90% of people with a specific condition are not following the prescribed treatment plan, I would suggest – in fact, I did suggest when I took the microphone – the problem is not with the people.
It is with the treatment. Of course it is with the treatment.
The problem with the language of adherence is that it frames outcomes through the lens of personal responsibility. It absolves policy makers of any duty to act and address the structural, economic and systemic barriers that prevent people from accessing and maintaining treatment. Why would they intervene and develop policy if the issue is seen as people being lazy or not committing to their health?
And it means the healthcare professionals are let off the hook. It assumes they are the holders of all knowledge, the giver of treatment and medications, and the person in front of them is there do what they are told.
There is no room in that model for questions, preferences, or complexity. There is no room for lived experience. There are no opportunities for co-design, meaningful engagement or developing plans that are likely to result in better outcomes.
When the room was opened up to questions, I raised these concerns, and the response from the emcee was somewhat dismissive. In fact, she tried to shut me down before I had a chance to make my (short) comment and ask a question. I’ve been in this game long enough to know when to push through, so I did. I also don’t take kindly to anyone shutting down someone with lived experience, especially in a session where our perspective was seriously lacking. Her response was to suggest that diabetes is different. I suggest (actually, I know) she is wrong.
And I will also add: while there was a person with lived experience on the panel, they were given two questions and had minimal space to contribute beyond that. I understand that there were delays that meant they arrived just in time for their session, but they were not included in the list of speakers on the flyer for the event while all the health professionals and those with organisation affiliation were. There comments were at the very end of the session, and I was reminded of this piece I wrote back in 2016 where health blogger and activist Britt Johnson was expected to feel grateful that the emcee, who had ignored her throughout a panel discussion, gave her the last five minutes to contribute.
Collectively this all points to a bigger issue, and we should name that for what it is: tokenism.
I didn’t point this out at the time, but here is a free tip for all health event organisers: getting someone to emcee who is a journalist or on-air reporter does not necessarily a good emcee make. Because when you have someone with a superficial understanding of the nuance and complexity involved in living with a chronic health condition, or understand the power dynamics and sensitivities required when facilitating a conversation about long-term health conditions, you wind up with a presenter who may be able to introduce speakers, but you miss out on meaningful and empathetic framing of the situation. There are people with lived experience who are excellent emcees and moderators, and bring that authenticity to the role. Use them. (Or get someone like Femi Oke who moderated the Helmsley + Access to Medicine Foundation session later in the day. She had obviously done her homework and was absolutely brilliant.)
I know that there has been a lot of attention to language in the diabetes space. But we are not alone. In fact, so much of my understanding has come from the work done by those in the HIV/AIDS community who led the way for language reform. There are also language movements in cancer care, obesity, mental health and more. And even if there are not official guidelines, it takes nothing to listen to community voices to understand how words and communication impact us.
So where to from here? In my comment to the panel, I urged the World Heart Foundation to reconsider the name of their campaign. Rather than framing their activities around adherence, I encouraged them to look for ways to support engagement and work with communities to find a balance in their communications. I asked that they continue to focus on naming the barriers that were outlined in the presentations, and shift from ‘How to we get people to follow?’ to ‘How do we work with people to understand what it is that they can and want to follow?’.
Finally, it was great to see International Diabetes Federation VP Jackie Malouf on the program on the panel. She was there to represent the IDF, but also brought loved experience as the mother of a child with diabetes. The IDF had endorsed World Adherence Day and perhaps had seen some of the public backlash about the campaign and the IDF’s support. Jackie eloquently made the point about how the use of the word was problematic and reinforced stigma and exclusion, and that there needs to be better engagement with the community before continuing with the initiative.
One of the things of which I am most proud is seeing how the language matters movement has really made people stop and think about how we communicate about diabetes. Of course, there’s still a long way to go, but it is very clear that there have been great strides made to improve the framing of diabetes.
One area where there has been a noticeable difference is at diabetes conferences. I’m not for a moment suggesting that there is never negative language used at conferences and meetings, but the clangers stand out now and are likely to be highlighted by someone (i.e. #dedoc° voices) in the audience.
Earlier this month, the 75th IDF World Congress was held in Bangkok. Sadly, there was no livestream of the Congress, but it’s a funny thing when you have a lot of friends and colleagues (i.e. #dedoc° voices) in attendance. It meant that I had my own livestream. Sadly, the majority of what I was being sent were the language clangers.
But let’s step back a week or so to before the Congress even started. I was feeling horrendous and my brain was in a foggy, virus haze, yet I still managed to be indignant and vent at the horrendously titled ‘World Adherence Day’ which was being ‘celebrated’ on 27 March. Here is my post from LinkedIn, which has been viewed close to 12,000 times:
What I didn’t say in my post was that the IDF had eagerly endorsed the day with a media release and social media posts. My LinkedIn post took all my energy for that day, and I didn’t get a chance to follow up with the IDF. Plus, I assumed their attention would have been focused very much on the upcoming Congress.
Also, I hoped that it was a one-off misstep. I mean, surely the organisation had learnt its lesson after the Congress in South Korea when I boldly challenged incoming-president Andrew Boulton for his suggestion that people with diabetes need some ‘fear arousal’ to understand how serious diabetes is. You can see the video of my response to that at the end of this post and read the article I co-authored (Boulton was another co-author) about language here.
Alas, I was wrong. Just days before the Congress started, I saw flyers for this session shared online:
I was horrified and commented on a couple of the posts I saw. I was surprised to see some responses from advocates which amounted to ‘We can deal with it when we get there.’ Here are reasons that isn’t good enough. Firstly – not everyone is there, so all they see is the promotional of an event, comfortably using stigmatising language. It suggests that this language and the meaning behind it is okay. The discussion shouldn’t be happening after the fact. In fact, the question we should be asking is: HOW did this even happen? Where were the people with lived experience on the organising committee of the Congress speaking up about this? Did they get to see it before it was publicised? And how did the IDF miss it? This is, after all, the organisation that launched a ‘Language Philosophy’ document in 2014 (which sadly seems to be unavailable online today). It’s also the organisation that has invited me to give a number of talks about the importance of using appropriate and effective communication to IDF staff, attendees of the Young Leaders Program and as an invited speaker at a number of Congresses.
A major sponsor at the IDF Congress seemed to be very excited about the word adherence. In fact, it appeared over and over in their materials at the Congress. Here is just a couple of their questionable messaging sent to me by people (i.e. #dedoc° voices) attending the Congress:
I will point out that the IDF obviously understands the impact of stigma on people with diabetes and the harm it causes. There were sessions at the Congress dedicated to diabetes-related stigma and how to address it. In fact, I had been invited to give one of those talks. But what is disappointing is that despite this, terminology that contributes to stigma is being used without question.
I wasn’t at the Congress but from what I saw there was indeed a vibrant lived experience cohort there. #dedoc° had a scholarship program, and, as usual, there was a Living with Diabetes stream. However, I will point out that the LWD stream was not chaired by a grassroots advocate as has been the case for all previous LWD streams. It was chaired by a doctor with diabetes and while I am in no way trying to delegitimise his lived experience, I am unapologetically saying that this is a backwards step by the IDF. When there is an opportunity for a person with diabetes who is not also a health professional is given to a health professional or a researcher, that’s a missed opportunity for a person with diabetes. There were seven streams at the IDF Congress. All except for one are 100% chaired by clinicians and researchers. Only the LWD stream is open to PWD. I know that when I chaired the stream, the four members of the committee were diligent about looking through the entire and identifying any sessions that could be considered problematic for people with diabetes. It appears that didn’t happen this time.
All of this points to a persistent disconnect. It is undeniable that the language matters movement is growing, but it is still not embedded across the board—even within organisations that should know better. If we are serious about addressing stigma and centring lived experience in diabetes care, then language can’t be an afterthought or a debate to have after the posters are printed and the sessions are underway. It must be part of the planning and the review process. The easiest way to connect the dots is to ensure the lived experience community is not only present, but also listened to, respected, and in positions to influence and lead. We are long past the point where being in the room or offered a solitary seat is enough – the room is ours; we are the table.
Postscript:
I have written extensively on why language – and in particular the word ‘adherence’ – is problematic. It’s old news to me and to many others as well. This piece isn’t about that. But if you want to know why it’s problematic, here’s an old post you can read.
Disclosures:
I was an invited to give a talk about diabetes-related stigma at the IDF Congress in Bangkok, but disappointingly, had to cancel my attendance due to illness. The invitation included flights and accommodation as well as Congress registration. I was also on the program for two other sessions and was due to present to the YLD Program.
Other IDF disclosures: I have been faculty for the YLD Program for the last 10 years; I chaired the LWD Stream at the 2019 Congress and was deputy chair of the 2017 Congress.
How was your Diabetes Awareness Month? I celebrated by taking a step back from most online activities and burying my head in the sand. Because, as always, Your Diabetes (Awareness Month) May Vary. #YDAMMV – get it trending!
I got COVID at the beginning of November and that was the definition of Not Fun. I was lucky in a lot of ways – I managed to take my first dose of anti-virals an hour after the ‘you’re positive’ lines came up on a RAT and was able to recover at home mostly. I easily accessed care when I needed it, and, in circumstances absolutely not normal for most, had heads of diabetes, and infectious diseases, departments at city tertiary hospitals calling to check in on me and make sure I had all I needed. (I know this is a perk of the work I do, and I recognise the remarkable privilege my work offers.)
I also spent November making some big life decisions and some big life moves (We’re in New York for the next three months) and that has all been kind of…big. I have never been so grateful of my incredibly supportive family and friends and, especially diabetes friends who have been an absolute bedrock on helping me through this time.
But here I am. It’s December. And it’s cold. December and cold are not words that generally go together for an Aussie sun-lover, but I am more than happy to be living in a city where Christmas carols suddenly make sense. Humming ‘Baby, it’s cold outside’ when the aircon is blasting, wearing a tank top, and sweating in 40°C heat is all sorts of oxymoron. This year, I’m wandering the streets in boots, a giant pompom adorning my beanie and wrapped in layers of coats and scarves, just as Mariah Carey intended.
Next week, I’m leaving New York and travelling to Lisbon for the IDF Congress. I’m so honoured to have been invited to give an Award Lecture, as well as speak in and chair a number of other sessions. The best part of this particular conference is the Living with Diabetes Stream which is dedicated to recognising diabetes lived experience. I can’t wait to hear from diabetes advocates from all over standing on stages and bravely, authentically and honestly sharing their stories. I wish more professional conferences had this sort of focus. And I also can’t wait to meet up with diabetes friends, some of whom I’ve not seen since before COVID. The Congress will be big and there will be a lot of it shared online. Keep an eye out!
Oh, and if you haven’t managed to get your #dedoc° voices scholarship application in yet, now is the time. The deadline has been extended by a few days and you have until next week to get yours in. You’d be mad not to, because become a #dedoc° voice means joining remarkable diabetes advocates from across the world and becoming part of a network like no other. Learning from dozens and dozens of people with diabetes who are there to do nothing but build community and support each other is incredible. Come join us! (Disclosure: I am Head of Advocacy for #dedoc°.)

One of my favourite memes on social media is the response to people who tell the world they’re taking a break from or leaving social media groups or platforms: ‘This is not an airport. There is no need to announce departures.’ (Aussie airports at the moment are full of cancelled flights, so departure announcements seem to be few and far between, but I digress.)
And so, I didn’t announce that I was taking a little break from the online world. It wasn’t really planned. But it has coincided with a couple of weeks break from work and it’s been nice to step away a little and just be. Plus, it’s given me a lot of time to write and write and write and smash deadlines for some of the freelance work I never seem to have enough time to get done. (My submission emails inevitably start with ‘I’m so sorry for the delay in getting this to you…’) But here on Diabetogenic, I’m the editor, so delays are only holding me up and it would be weird to apologise to myself for repeatedly missing deadlines, especially when I don’t even have deadlines (mostly because I don’t set them because I know I’d never meet them) and there I go digressing again and is it any wonder I get nothing done?!
Having said that, I’ve received dozens of emails from people asking when to expect a new post, so to everyone who has messaged or wondered: ‘I’m so sorry for the delay in getting this to you…’.
But here I am back again, with a heap of great things I’ve seen recently and I want to share them here in a bit of an interweb jumble!
I’m writing
Yes, I know it’s weird to share my own writing on my own blog, but whatever! Plus,, there is nothing wrong with a bit of self-promotion. I’m back writing for diaTribe and absolutely delighted to have had these two pieces published recently.
This one is about how it’s important to tell stories of people with diabetes who choose to not run marathons or climb mountains in amongst stories of those who do.
And this one is about a new type 1 diabetes screening program for Australian children. I write about the reservations I had about having my daughter screened when she was little, but how things might be very different with research like this. The response to this article has been lovely and a lot of parents with diabetes have reached out to say that they have had similar concerns and feelings to those I articulate in the post.
Advocacy through art
I’m a huge fan of Jenna Cantamessa’s artwork, and this beautiful image and accompanying post is one of the reasons why! Click on the artwork to be taken to the TypeOneVibes Instagram account to read Jenna’s words.
Stripped Supply
I’m always happy to promote smart women doing smart things and so let me introduce you to Ashley from Stripped Safely.
When Ashley’s boyfriend was diagnosed with type 1 diabetes, she realised there was a gap in the market when it comes to mail ordering NDSS supplies. Remember the old days when we used to be able to easily place an order online and have our pump lines or BGL strips delivered straight to our front door? Well, Ashley is making that happen again. It’s a subscription service and is super easy to use. Details about how to use Stripped Supply here.
Gong
You bet I’m proud to share this! Diabetes Australia’s Heads Up on Diabetes campaign recently received an award from the Australian Patients Association. The campaign was recognised as the Best Patients’ Campaign and how wonderful that shining a spotlight on diabetes and mental in such a powerful way has been awarded.
I’ll just say that while it is truly amazing to be acknowledged in this way, the real measure for me of the success of a campaign is how the diabetes community responds and it was clear from year one of this three-year campaign that people with diabetes from across the world absolutely loved it, as evidenced by the number of times the campaign videos were shared online. Oh, and there’s something quite incredible about sitting in a conference room and seeing our work played back to us by someone from outside the organisation. Yeah – that’s happened a number of times!
The Human Trial
So much buzz in the diabetes world at the moment about the incredible documentary out of the US, The Human Trial. Until 9 September, you can stream the film for free by going to this link. You will be prompted to make a donation if you can. All funds raised go to diabetes research.
More about this documentary soon.
Advocacy through poetry 1
At the recent Australian Diabetes Congress, I had the honour and pleasure of chairing a session with an brilliant array of diabetes advocates from Australia and across the world. One of the speakers was Ash Byrne who began her presentation with an incredibly powerful poem and then went on to speak about the mental health burdens of diabetes. You can see Ash readying her poem, Invisible, at this Facebook link.
Advocacy through poetry 2
Aussie diabetes advocate and #dedoc° voice, Leon Tribe shared this poem on Twitter earlier this week which beautifully explains the power of language and communication between people with diabetes and our healthcare professionals. (You may need to click on the image to read the poem more easily.)
Stigma – diabetes and beyond
‘I have a new thing, and I didn’t want to talk about it. In part, because of stigma. Mostly, because of stigma.’
This is the start of a powerful post from Dana Lewis where she shares how the stigma that comes with diabetes has influenced how she feels about being diagnosed with another autoimmune disease. Read it here.
TEDx does diabetes advocacy
I’ve been a long-time fan of Grainne Flynn’s advocacy work and have shared her posts here before. Recently, she did a TED Talk about grassroots advocacy. It is all shades of brilliant and an absolute joy to watch. So… watch!
#dedoc° is busy!
There is a lot going on in the world of #dedoc°! Here’s just a taste of upcoming events that everyone can get involved in. Plus, the #dedoc° voices program will be kicking off again later this month at EASD with a cohort of new voices and alumni on the ground in Stockholm as well as following along virtually.
I’m so excited to be part of the #dedoc° symposium at EASD! Delivering a community led and focused symposium as part of the scientific program at a professional is a Big.Deal. We’re continuing to live and breathe #NothingAboutUsWithoutUs in the most impressive ways!
Disclosures
As always, I am thrilled to share things that I’ve found interesting, but disclosures are important. I’ve not been asked to share anything you see here, but figure if I find something interesting (or feel like doing same shameless self-promotion) you might too. I also figure that being transparent is important as is reminding you to consider my bias when sharing things.
- I am a paid contributor to diaTribe
- I am the Head of Communities & International Affairs at Diabetes Australia
- I am the Global Head of Advocacy at #dedoc°
Psst…forgotten something?
If you’re in the northern hemisphere right now, you’re possibly all caught up in the sunshine, splashing around at the beach or spending time off work just taking time out. If you’re from the southern hemisphere, you’re either smart and have taken a holiday to Europe because EVERYONE.IS.IN.EUROPE.RIGHT.NOW, or under fifteen quilts in front of a roaring fire, counting down the days until it gets warmer. Sadly, I’m in the latter group.
I get it. Things slip by either way.
But! You only have a few days left to make sure you don’t miss out on applying for a #dedoc° voices scholarship. Wherever you are, a scholarship means you have something to look forward to in a couple of months’ time and the absolute thrill of either virtually or in-person attending a global diabetes conference or two. That’s right – TWO! EASD (European diabetes conference) and ISPAD (paediatric diabetes conference) are the next international conferences on the diabetes conference calendar. Both will be hybrid, with the in-person locations being Stockholm and Abu Dhabi respectively.
We’re well over two years into the #dedoc° voices program now, and the awesome thing about it is that it’s not just about the few days of the conference where you get to learn from incredible researchers and clinicians, while waving the lived experience flag and being surrounded by others with diabetes. I mean, that is all pretty great. But being a #dedoc° voice goes way beyond that! Once you receive a scholarship you are part of a network of remarkable diabetes advocates from across the world, and this network is the most supportive, encouraging, brilliant group of people, always ready to help. Every single week, I see people reaching out for support and advice and the responses are swift and many. I’ve not seen a single example of anything other than support, and have watched advocates truly flourish as they have worked with others, developed mentoring relationships and been supported to do brilliant things.
Unless you’re part of the program, you wouldn’t know this. And here’s the deal: anyone can become part of it. The #dedoc° voices program is open to people from across the world and everyone is in with an equal chance. You just need to spend some time completing an application. It is a competitive process, and places are limited. The people who get accepted are the ones who have taken some time with their application and really been able to demonstrate just how they are going to #PayItForward to their diabetes community if successful. No one is a shoe in; having a high follower count on socials means nothing if your application is sub-par. We take people who are new to the diabetes advocacy space, and are looking for a hand carving out their space, as well as seasoned advocates who are keen to work with others and become part of a global network, outside their own country.
So, get on it! Click on the image below, fill in the form and join us! You get to work on your advocacy while giving back to the community, all while wearing the #NothingAboutUsWithoutUs badge. How amazing is that?!
More on #diabetogenic about the #dedoc° voices program:
#dedoc° voices helping people with diabetes get into professional conferences
How #dedoc° voices supported people with diabetes in Ukraine
More on why to apply to join the #dedoc voices program
Disclosure
I have been an advisor for a number of years, and am now working with them as Head of Advocacy.
I don’t know what I was expecting, but I was thinking that diabetes conferences in the time of COVID would be different to pre-COVID times. But really, apart from some people wearing masks, less kissing the cheeks of strangers and sharing vaccination status (‘How many times have you been boosted?’), there wasn’t all that much the differed from the last face-to-face conference back in February 2020.
I realised that on day 2 as I walked through the barely light streets of Barcelona from my hotel to the conference centre that the idea and demands of ‘conferencing hard’ hadn’t changed. The 6.30am breakfast was still alive and well, scheduled so that there was time for another morning session before the actual sessions started. It makes for a very long morning which is what I said walking out of my fourth meeting for the day and seeing it was still only 10.30am.
Also the same is the way conference session timetablers still manage to clump all the sessions I want to go to in the same time block! I barely made it to any sessions anyway, (project and collaboration meetings made it difficult), but when I did have a spare half hour there were always several concurrent sessions I wanted to be in.
And in the same way, there is a magical equation applied to room allocation that results in the most popular sessions being given the smallest rooms, so that people are crowded in and then overflowing – something that has always been a problem but seems even more of an issue in COVID times.
The Exhibition Hall remained a playroom for HCPs with ever brighter and flashier booths all vying for attention. In what is starting to resemble a Las Vegas casino room, blinking lights, interactive boards, and promising giveaways keep attendees away from sessions and focused on shiny work of overpaid marketing and PR firms. They earn their coin – There were queues outside the Exhibition Hall each morning, and the booths were jam packed throughout each day.
I had one of the most confusing and weird experiences ever in this Exhibition Hall at the Abbott stand. I’d been given a heads up that they were giving away dummy Libre 3 sensors on the stand, so I wandered over to see what the buzz was all about. All around the massive booth that had prime position right at the entrance of the hall were giant interactive screens. Attendees were invited to work their way through a six-question survey to test their knowledge on Freestyle Libre 3.
After I got my score, I walked up to one of the Abbott staff and we had this encounter:
Me: ‘Hi, I’ve just done the survey and I was wondering if I could get a dummy sensor, please.’
Abbott staff: ‘I’m sorry?’
Me: ‘Oh, um… a demo sensor?’
Abbott staff: ‘We don’t give away demonstration sensors. Health professionals can register to have one sent to them.’ (She was eyeing the N/P label on my badge.)
Me: ‘Okay, well we can talk about that another time, but for now, what is the sensor that is being offered to people finishing the survey thing? A dummy sensor?’
Abbott staff: ‘Oh no. we don’t have dummy sensors. We have … (pause for effect) … glamour sensors.’ She wandered off to get me one while I stood there stunned at what I had just heard.
Look, I know I spend a lot of time working in the space of diabetes and language, but this one had be absolutely floored. Glamour sensor? I turned to my friend Andrea who had watched this entire encounter and we both mouthed in astonishment ‘Glamour sensor?’
The Abbott rep returned and handed me a box that looked suspiciously like it contained an engagement ring, which I thought was lovely if not a little forward considering we’d only said half a dozen sentences to each other.
I thanked her and opened it and there inside was this:

I sighed. There was my glamour sensor. A fun little token of love from the device company that makes a bloody good product…that is unaffordable to the vast majority of people with diabetes who could benefit from it. I get the excitement though. It is very sexy. It’s tiny and obviously I desperately want it to come to Australia NOW so that we can have access to it. Thank you and please. But is the fanfare and theatre around it at a diabetes conference all that necessary?
Which brings me to another thing that is exactly the same. As I get swept up in the excitement of new technology much like anyone else, I have another focus. And that focus is horribly annoying for whichever rep asks if they can help me when the see me lurking with intent at their booth. ‘Nice kit,’ I say to lull them into a false sense of security, letting them think I am just like any other admiring punter wandering around. And then: ‘When is it coming to Australia?’ The answers are always the same – no matter who I am speaking to and no matter which company they are from. It’s a variation on ‘No idea; maybe I do know, but I can’t tell you; you’re a long way away; there aren’t many of you; stop asking me.’
Also slightly gimmicky, but absolutely for the right reasons, was the demo Omnipod give away at the Insulet stand. Here, anyone could simply head up to the stand and ask for one, and Insulet would make a €5 donation to Spare a Rose for Ukraine. I can’t really complain about this seeming like a stunt when it’s going to a cause very, very close to my heart…!!
One of my favourite things that was a throwback from pre-COVID conferences was seeing groups of people with diabetes – many there as part of #dedoc° voices – wandering around together in packs, comparing notes, and supporting each other. That is something that certainly hasn’t changed, other than for those packs to be more recognisable and more welcome. Definitely a good thing! And something that I hope to see a lot more of in coming meetings.
DISCLOSURE
My flights and accommodation have been covered by #dedoc°, where I have been an advisor for a number of years, and am now working with them as Head of Advocacy.
Thanks to ATTD for providing me with a press pass to attend the conference.
Throughout ATTD I got to repeatedly tell an origin story that led us to this year’s #dedoc° symposium. I’ve told the story here before, but I’m going to again for anyone new, or anyone who is after a refresher.
It’s 2015 and EASD in Stockholm. A group of people with diabetes are crowded together in the overheated backroom of a cafe in the centre of the city. Organising and leading this catch up is Bastian Hauck who, just a few years earlier, brought people from the german-based diabetes community together online (in tweet chats) and for in person events. His idea here was that anyone with diabetes, or connected to the conference, from anywhere in the world, could pop in and share what they were up to that was benefitting their corner of the diabetes world. I’ll add that this was a slightly turbulent time in some parts of the DOC in Europe. Local online communities were feeling the effects of some bitter rifts. #docday° wasn’t about that, and it wasn’t about where you were from either. It was about providing a platform for people with diabetes to network and share and give and get support.
And that’s exactly what happened. Honestly, I can’t remember all that much of what was spoken about. I do remember diabetes advocate from Sweden, Josephine, unabashedly stripping down to her underwear to show off the latest AnnaPS designs – a range of clothing created especially to comfortably and conveniently house diabetes devices. It won’t come as a surprise to many people that I spoke about language and communication, and the work Diabetes Australia was doing in this space and how it was the diabetes community that was helping spread the word.
I also remember the cardamom buns speckled with sugar pearls, but this is not relevant to the story, and purely serving as a reminder to find a recipe and make some.
So there we were, far away from the actual conference (because most of the advocates who were there didn’t have registration badges to get in), and very separate from where the HCPs were talking about … well … talking about us.
Twelve months later EASD moved to Munich. This time, Bastian had managed to negotiate with the event organisers for a room at the conference centre. Most of the advocates who were there for other satellite events had secured registrations badges, and could easily access all spaces. Now, instead of needing to schlep across town to meet, we had a dedicated space for a couple of hours. It also means that HCPs could pop into the event in between sessions. And a few did!
This has been the model for #docday° at EASD and, more recently, ATTD as well. The meetups were held at the conference centre and each time the number of HCPs would grow. It worked! Until, of course COVID threw a spanner in all the diabetes conference works. And so, we moved online to virtual gatherings which turned out to be quite amazing as it opened up the floor to a lot of advocates who ordinarily might not be able to access the meetings in Europe.
And that brings us to this year. The first large international diabetes conference was back on – after a couple of reschedules and location changes. And with it would, of course, be the global #dedoc° community, but this time, rather than a satellite or adjacent session, it would be part of the scientific program. There on the website was the first ever #dedoc° symposium. This was (is!) HUGE! It marks a real change in how and where people with diabetes, our stories and our position is considered at what has in the past been the domain of health professionals and researchers.
When you live by the motto ‘Nothing about us without us’ this is a very comfortable place to be. Bastian and the #dedoc° team and supporters had moved the needle, and shown that people with diabetes can be incorporated into these conferences with ease. The program for the session was determined by what have been key discussions in the diabetes community for some time: access, stigma and DIY technologies. And guess what? Those very topics were also mentioned by HCPs in other sessions.
There have been well over a dozen #docday° events now. There has been conversation after conversation after conversation about how to better include people with diabetes in these sorts of events in a meaningful way. There has been community working together to make it happen. And here we are.
For the record, the room was full to overflowing. And the vast majority of the people there were not people with diabetes. Healthcare professionals and researchers made the conscious decision to walk into Hall 118 at 3pm on Wednesday 27 April to hear from the diabetes community; to learn from the diabetes community.
If you missed it, here it is! The other amazing thing about this Symposium was that, unlike all other sessions, it wasn’t only open to people who had registered for ATTD. It was live streamed across #dedoc° socials and is available now for anyone to watch on demand. So, watch now! It was such an honour to be asked to moderate this session and to be able to present the three incredibly speakers from the diabetes community. Right where they – where we – belong.
DISCLOSURE
My flights and accommodation have been covered by #dedoc°, where I have been an advisor for a number of years, and am now working with them as Head of Advocacy.
Thanks to ATTD for providing me with a press pass to attend the conference.