You are currently browsing the category archive for the ‘Conferences’ category.
Over the weekend, an embargoed press release arrived in my inbox with a few different pieces of research that would be presented in coming days at EASD.
Being registered as press for diabetes conferences means getting an advance peek into some of the big stories that are likely to generate a lot of interest and discussion. This email offered three or four pieces of research, but it was the first one listed in the subject heading that made me catch my breath and hesitate on the button to read the email beyond the header,
Shorter. Life. Expectancy.
The three words ran through my mind over and over before I steeled myself enough to open the email and read the release, then the abstract and finally the full article. As confronting as the email header was, there was nothing in there that I didn’t expect, and nothing really that surprised me. It’s not new news. I remember being told early into my diagnosis that I could expect to live 15 years less because of diabetes; something I casually announced to my sister one night when we were out for dinner. Through tears, she made me promise to never say that again, and I just hope she’s not reading this right now.
But even though there was nothing in there that made me feel especially concerned, I did bristle at the conclusion of the article, in particular this:
‘Linking poor glycaemic control to expected mortality … may incentivise … people with diabetes and poor control to increase their efforts to achieve targets.’
I’m ignoring the language here, because even more problematic than the specific words in here is the sentiment which I read as ‘scare people and threaten them with early death to try harder’. Unsurprisingly, I find that horrendous. Equally horrendous is the assumption that people are not already trying as hard as they possibly can. It’s not possible to increase efforts if someone is already putting in the maximum.
Over the last twenty-two years, my diabetes management has sat at pretty much every single data point along the ‘glycaemic control’ spectrum, from A1Cs in the 4s and 5s all the way up to the mid-teens. There is no way that being told that I was going to die earlier would have made me pull up my socks to do better. In fact, it’s likely that if anyone had, at any point (but especially when I was sitting way above target), told me that I was sending myself to an early grave, all that would have done was send me further into the depressive burnout hole I was already cowering in.
It’s tough going knowing that the health condition that I’m doing everything in my power to manage as best as I possibly can is going to contribute to cutting my life short; that despite those efforts, I am likely to see fewer years of my daughter’s life and be outlived by most of my friends. Placing any of the blame for that on me for that makes me feel even worse.
I’m not here to argue with the article – it was an analysis of an audit of data out of England. I’m not here to say that this sort of information shouldn’t be shared, because of course it should be. Understanding outcomes, what drives them, interventions that can help and any other factor that provides better results for people with diabetes is a brilliant thing. These sorts of results could be used to highlight when and how to intensify and prioritise treatment options.
I do, however, question the way that the information will be used. Also, from the article:
‘Communication of life years lost from now to patients at the time of consultation with healthcare professionals and through messages publicised by advocacy groups … and … national/international patient facing organisations will be of great help in terms of disseminations of the conclusions of this study.’
I would be really dismayed if I saw any diabetes organisation using this information in a comms campaign, as I fear it could add concern and trauma to people living with diabetes. I worry about how it could be interpreted by well-meaning loved ones to say, ‘If you don’t start looking after yourself, you’re going to die,’ or something similar.
For the record, one of the other studies highlighted in the email was about hot baths and diabetes. The lowdown on that is having regular hot baths may improve cardiovascular risk factors in people with type 2 diabetes. I’m going to do an n=1 study to see if that also helps people with diabetes.
This week, it’s EASD. It’s is the first year since 2012 that I have not been in Europe for the meeting. EASD was the first large diabetes professional meeting I had ever been to, and I remember being struck at that very first one in Berlin by the stark absence of people with diabetes on the program and involved in the actual meeting.
My, how things have changed.
Except, of course, they haven’t. Sure, these days you will see growing numbers of PWD wandering the conference centre and attending sessions, but that really is only because we created opportunities for PWD to attend. And once we found a way to get there, we then made sure that we were visible in different ways such as leading social media charges and holding events open to all attendees.
There has been some very well placed and relevant conversation on twitter about the lack of diversity in the EASD organising committee. Too few women; too many white faces. But when we talk about inclusion, surely, surely we need to look at other groups that are significantly and obviously absent. Where are the advocates on there? Where are the BIPOC with diabetes? Where are people living with both diabetes and disabilities? Where is there representation from the diabetes LBGTIQ community? All of these factors impact on diabetes management, so wanting to see presentations that address them makes sense. And where is the lived experience on the program to underline, and provide real relevance, to the work that is being presented by HCPs, researchers and academics?
You bet there should be more women and more BIPOC on the organising committee for EASD. But if those on the committee, those doing the research, those HCPS seeing PWD truly want to beat the ‘person-centred’ drum, PWD need to be part of the group of people putting the conference together, and then strongly represented on the stage too.
#NothingAboutUsWithoutUs seems to STILL be missing from this whole meeting – from the organisation right through to the actual delivery of information. (I suspect that there may be some PWD on the program who are HCPs. While that is terrific, it is very different from having advocates who are not HCPs up on stage.)
So, this week, if you can, please support initiatives that do highlight the people who are actually living with diabetes. Please check and double check the times. I’ve tried to work out the AEST start time for all of the events, but don’t take my word for it! (Disclosure statement at the end of this article.)
#docday° & #dedoc° voices
This is the eleventh (I think??) #docday° event and I am so proud to say that I have been involved in every single one of these events. The first one was held in the back room of an overheated and overcrowded café in Stockholm five years ago. It feels like yesterday, and a lifetime ago all at once. Organiser, Bastian Hauck, asked me to say a few words, and this is what I wrote in a blog post about the event:
‘I highlighted for me what is the most important thing when we are talking about the DOC: No one owns this community. No one is more important or more relevant or more powerful. Sure, some of us are very fortunate that we get to actually meet IRL and attend conferences, but we do it as part of our jobs – whether it be like me (through my work at a diabetes organisation mixed with my online work) or through independent consulting or other work. But regardless if you are in the room or following along on Twitter, everyone has the same right to be here and to be part of it.’
We have livestreamed #docday° events in recent years, and I have written about most of them, and done all I could to encourage as many people as possible to come along and join in. This year, it will once again be livestreamed from the #dedoc° Facebook page from Tuesday (today) 12pm CET tonight, which is 8pm AEDT.
Also, make sure you keep an eye out for all the terrific advocates who received a scholarship to attend EASD via the #dedoc° voices program. They are sharing what they are seeing at the meeting on a variety of social platforms.

SOLVABLE PROBLEMS IN DIABETES
A few hours later, diaTribe will be continuing the Solvable Problems in Diabetes events which have been regular satellite events at European diabetes meetings in recent years. During COVID times, these events have been kicked off with a community focus event, showcasing diabetes advocates, which is a brilliant (and necessary) addition to the HCP discussion that follows. I’m a huge fan of diaTribe, and have been for a long time, but it has been the addition of Cherise Shockley to their team as Community Manager that has seen a wonderful increase in representation of PWD in their activities. But, of course it has. Cherise is all about community and the way she has been able to weave her magic to make diaTribe even more relevant to PWD – and more representative – is what she does best. You’ll need to register for this event (it’s free) here, and it kicks off at Tuesday 11.30am ET, which is (gulp) Wednesday 1.30am AEDT.

SEPTEMBER SESSIONS
While not part of EASD, Beyond Type 1 is hosting the next in their Summer Sessions and this week it’s focusing on racial and ethnic disparities in diabetes care. There is an absolutely stellar line up in this webinar. Please do follow along if you can – this event will also be via Facebook Live over at Beyond Type 1, and is on Wednesday 8pm ET, which is Thursday 10am AEST.

DISCLOSURES
- I am ad advisor to the #dedoc° voices program. I do not receive any payment for this role.
- I am speaking at the Solvable Problems in Diabetes Community Focus Sessions. I am not receiving any payment for my involvement. I am a regular contributor to diaTribe, and I am paid for commissioned articles.
- I am on the Leadership Council for Beyond Type 1. I do not receive any payment for this role.
Diabetes conferences and scientific meetings in 2020 have looked very different than in previous years. It looked as though we were off to a flying start with a successful ATTD in Spain back in February. But not long after all the attendees returned to their corners of the globe, the world turned upside down and decided that, along with everything else, in-person meetings were done.
Major professional conferences such as those run by ADA, DUK, EASD, ISPAD, ADS & ADEA and IDF have all either happened, or will be happening, virtually, with a Zoom (or other) platform being where we meet, rather than a massive conference centre in a major city.
As ever, I search for a silver lining and if there is one it is this: the pivot to virtual conferences means that some of the main barriers in the way preventing PWD attending diabetes conferences are somewhat reduced. With travel, accommodation and a lot of the other expenses out of the way, it may be easier for advocates who would like to attend to find their way in. Let’s look at that as the disruption we needed to have to get PWD flocking to meetings in droves.
There is still the matter of registration passes, and we know that is not always the easiest thing to overcome. The registration fee is significant, and some conferences only allow HCPs and researchers in. Usually, press passes provide a way to get passed security, but they require letters of assignment (sometimes from diabetes organisations who ask PWD to act as ‘on the ground’ reporters), or other criteria be met. And, of course, there are invitations to attend satellite events extended from device and drug companies to some advocates. While there is often criticism at these methods, they have meant that there are PWD at conferences, many of whom provide information back to the community.
At ATTD, there was a new way in. Advocacy group #dedoc° launched a new program, #dedoc° voices, which you can read all about here. For the pilot of the program in Madrid, the diabetes advocates whose applications were successful had access to all parts of the meeting.
#dedoc° voices is happening again for EASD (coming up next month), and it’s not too late to apply. And as an added bonus, successful applicants will also receive registration to the ISPAD conference in October. ISPAD is the International Society for Pediatric and Adolescent Diabetes, so if you are a parent of a kid with diabetes involved in advocacy and peer support, you may be super keen to attend this one.
To apply, go here. #dedoc° voices is open to PWD now, so if you have always wanted to attend a major diabetes conference, there is nothing stopping you from applying, right now. Any one from anywhere around the world can apply – the only consideration is how you’ll manage time zone horrors if you don’t live in the same zone as the conference. (But please don’t come crying to me about that – I’ve spent the last six months settling in for hour long meetings hosted out of Europe of the US which begin long after sunset and involve perky people just waking up while I yawn and struggle not to fall asleep in my Zoom square!)
What are you waiting for? Apply now and come be a part of one of the biggest diabetes meetings in the world. I promise there will be lots of other PWD there for you to (virtually) meet up, and share ideas with. Come say hi!
Disclosure
I am an advisor to the #dedoc° voices program. I do not receive any payment for this role. 
Sometimes it feels as though discussions in the diabetes are seasonal. Like clockwork, we see the same conversations happen at the same times. Without missing a beat, almost as soon as a scientific conference is over, someone will comment about how difficult it is for PWD to get to conferences (true, however this year, #dedoc° voices could have assisted a number of the people who were stating that), and then there are discussions about disclosure by PWD who are fortunate to attend, even though pretty much every advocate I know who attends these sorts of things does a stellar job of disclosing.
And of course, the nature of the first big meeting of the year, ATTD, means that there inevitably will be noise about the gap in technology access. And you bet this is a discussion that we need to be having on regular rotation.
After attending my first ATTD, I wrote a piece about the complete and utter dichotomy of being at a conference that was only talking about the latest and greatest in technology while, at the same time, whilst the community was in the midst of its usual Spare a Rose month of fundraising. I struggled to balance the idea that we were talking about automated insulin delivery at the same time as urging donations so people could just get insulin!
Today, I’m revisiting the piece I wrote after last year’s ATTD, where my worlds of diabetes technology and language matters merged, and combined this with the over-representation of those at the super-dooper-tech-y end of the diabetes technology spectrum. (‘Super-dooper-tech-y’ is, obviously, a very technical term.)
I don’t for a moment think that meetings with a strong tech focus should end, or that those who are innovators in technologies should take a seat and let others speak. I don’t believe that at all. I will be forever grateful to the pioneers who continue to push the envelope and make things better for people with diabetes. But I do think that we need to ensure that there is equal attention to those who – by choice or because of their circumstances – are not walking around with an algorithm driving their diabetes.
If we truly believe that all diabetes stories matter, then we need to hear from people doing diabetes in every way possible. Perhaps if we make more of an effort to find and hear those stories, we will stop minimising our experiences, and starr seeing that whatever we are managing to do is truly enough…
DISCLOSURE 1 (for ATTD 2020)
I was an invited speaker at #ATTD2020, and my registration was covered by the conference organising committee. My airfare and part of my accommodation to attend ATTD was covered by Lilly Diabetes so that I could participate in the DOCLab advisory group meeting which took place on Friday, Saturday and Sunday. Other accommodation was covered by DedocLabs (I am an advisor for the #dedoc° voices program) and Novo Nordisk (I am a member of DEEP). I have not been asked to write or speak about any of the activities I attended, or anything I have seen at the conference.
We all do a good job at undermining ourselves at times. We use a four letter word that diminishes what we are doing, and limits the value of our experience and expertise. That four letter word is ‘just’.
In diabetes, we hear it all the time: ‘Oh, I just have type 2 diabetes’ as though it is insignificant and doesn’t have any challenges. ‘I’ve lived with diabetes for just a couple of years’ because we think there is only currency in decades of living with the condition, when really any length of time with diabetes is meaningful.
And we are all about minimising our experience when it comes to the treatment of our diabetes. ‘I just use diet and exercise to manage my type 2 diabetes’ or ‘I’m just on tablets’ or ‘I’m just on injections twice a day’ or ‘I’m just on MDI’. The list goes on and on. And on.
I realised just how ridiculous we have become with this when I heard myself, during a conversation with a fellow Looper, ‘Oh, I just use Loop’. (More on that later…)
At the Ascensia Social Media Summit at ATTD we spoke about this, specifically how there is almost a stigma within the diabetes for those seen to not be using the shiniest and brightest and newest of technologies. It seems that some people almost feel embarrassed if they are not constantly updating their technology toolkit with the most recently launched product.
The idea that anything that we are using today is ‘yesterday’s technology’ is wrong. Blood glucose monitoring can’t be ‘yesterday’s tech’ if it is what most people are using to track their glucose. And syringes and pens can’t be considered the ‘old way to deliver insulin’ when that is how the vast, vast majority of inulin-requiring people with diabetes get insulin into their bodies. Plus, every single one of us using a pump must be able to deliver insulin this way because machines break.
Somewhere in discussions about our treatment technologies, we seem to have forgotten that, actually, not everyone wants to be using the latest kit. And that is okay. There is a spectrum of diabetes technology, and as long as we are on it somewhere and managing our diabetes the way that works best for us, then elephant stamps all around!
There is clearly an over-representation of people at one end of that spectrum dominating on and off line conversations. Spend a couple of hours in a diabetes Facebook group and it would be a reasonable assumption that most people are wearing pumps and CGM. But that’s not true.
And it could appear that DIYAPS is the way to go for most people with T1D, when the fact is that numbers are relatively low. It’s hard to estimate exactly, but there may be somewhere between 2,000 and 3,000 worldwide how have ‘built their own pancreas’. That is just a drop in the type 1 diabetes ocean.
It’s fantastic for those of us interested in this technology to be able to (virtually) congregate and talk amongst ourselves. I learn so much from my peers in these groups – just as I have with all aspects of life with diabetes. The lived experience continues to trump any other way of learning about diabetes.
Of course, that doesn’t mean that we shouldn’t be talking about technology used by limited numbers. Of course we should. We want others to know about it so they can make an informed choice about whether it may be right for them. We want our HCPs to know about it and to support those of us using all sorts of technologies and treatments.
Where it becomes problematic is when there is the misconception that this is the norm. Or when those not using the newest technology feel that they are wilfully doing diabetes the ‘old way’. It’s unfair to think for a moment that those who are not using the tech ‘don’t care’ enough about themselves – especially when decisions are made based on a very good understanding of what is available and what they have decided works best for them.
So, back to my ‘Oh, I just use Loop’ comment. It was directed to someone far more technologically advanced than me; someone who runs all sorts of other programs alongside their DIYAPS. They generate lots of reports and make lots of changes and seem to have far more bells and whistles than I even knew were available.
I nodded as they told me all they were doing and then, when they asked me how I manage my diabetes, I answered that I just use Loop. I heard myself saying it and stopped and corrected myself. ‘I mean…I use Loop. It works for me. Perfectly.’
We don’t need to make excuses for doing diabetes our own way. If we truly have choice (which I know is not always the case), and we have made the choice based on what we believe to be the best possible treatment and technology for us at that moment, then surely that’s a great thing. We shouldn’t ever be made to feel less committed to our own health and wellbeing. That’s not how it works.
DISLCOSURE 2 (for ATTD 2019)
I was invited by Ascensia to co-chair the Diabetes Social Media Summit at ATTD (#ATTDDSMS). I did not receive any payment or in-kind support from them for accepting their invitation. I have co-written a piece for the blog, however this was not edited (apart from inevitable jet-lag-induced typos) and all words are those of mine and the piece’s co-author. You can read that piece here.
When I first started working for a diabetes organisation, the first big project I oversaw was the development of a booklet providing information to young people living with type 1 diabetes. After approaching a few others out in the community working with and supporting this cohort, I was promptly reprimanded by one person who told me in no uncertain terms that I (and the organisation I was working for) should butt out, because this was not our space; it was this group’s area. I was somewhat astonished at the idea of ‘owning’ a segment of the diabetes community. How did that happen? Who decided that? I was a young person with type 1 diabetes at the time (obviously, this was years ago!), and I didn’t feel especially well-represented by any one group, and I certainly objected to the idea of someone deciding that their group spoke for me and my ilk.
The diabetes community is made up of many, many voices (some louder than others), and each person has different priorities for their own diabetes, and the broader issue of diabetes in general. We see that every day with different campaigns that are driven by people in the community. Some of the most visible are movements or campaigns that employ hashtags such as #Insulin4All, (although the insulin affordability discussion encompasses more than just this hashtag), #NothingAboutUsWithoutUs and #WeAreNotWaiting, and, as we are still in February, #SpareARose. (Not too late to donate, folks!)
Actually, #SpareARose is an excellent example of this. It may have been started by a few incredible advocates, but they never felt the need to identify themselves as the ones who led or created it. They encouraged anyone and everyone to be involved in any way they could – to donate, to share, to write about it, to make vlogs. It is owned by all and by no one at the same time!
At ATTD last week, Chris ‘The Grumpy Pumper’ Aldred and I took to the stage to do a presentation on #TalkAboutComplications, which incorporates the under-discussed issue of diabetes-related complications and its intersection with #LanguageMatters. Our talk was in a session that incorporated presentations focusing on peer support and diabetes online community and technology – all very much ‘user-led’ initiatives and movements.
These campaigns are not about everyone having the same idea and perspective. People approach different issues in different ways. One person’s peer support ideal is another person’s living nightmare! And #LanguageMatters remains a topic with myriad ideas and expectations for just how embedded it should be in the hearts and minds of our community and beyond.
But it is undeniable that no one really claims ownership of any of these movements. While Grumps may have tweeted that hashtag #TalkAboutComplications first, I know that he doesn’t feel that he ‘owns’ it, or discussions around it. Rather, he used it as a rallying cry to bring people together – to find a tribe, so to speak, and to connect people with diabetes searching for information and support about the realities of living with diabetes-related complications.
I (and a couple of others) have been accused of claiming ownership of #LanguageMatters because of our frequent posts, tweets and other commentary on the issue, but anyone who has aimed that accusation at me has either never heard me speak about the topic or read this blog. Whilst I may be extraordinarily proud that I work for the organisation that developed and launched the first position statement addressing this topic, and I have been invited to speak about our work a number of times, I very clearly point out the origin story of this movement, and that is very much a story from the diabetes community.
People with, or affected by, diabetes have been speaking about how words and language impact for a long time. Older online discussion boards frequently held debates about PWD/diabetic for as long as I have been diagnosed (and I’m sure, many years before that). Parents of kids with diabetes shared how they felt judged and shamed by the words used by HCPs when their kids A1Cs were out of range, feelings echoed by adults with diabetes.
I remember one of the first articles I read in Conquest magazine (Diabetes Australia’s magazine back when I was diagnosed) was by Gordon Bunyan who eloquently wrote about how words matter. Gordon has become a good mate, and over the years I’ve turned to him regularly to talk about this issue. And I remember hearing how teenagers at camps instigated change when it came to the language used when talking about glucose levels, moving from using good and bad, to the more factual high and low. That was back before I was working for the organisation involved in those camps.
Diabetes Australia, in developing that position statement, wasn’t sticking a flag in the issue, claiming ownership – and nor have any of the people involved in its development. It was a response to something that mattered to people living with diabetes – people who told us repeatedly that the words spoken to and about them, the attitudes that those words conveyed and the feelings they had when different words were used had the ability to empower or harm.
Having organisations build programs, activities, resources and services around what people affected by diabetes are talking about unites the community. It also demonstrates a willingness to listen and acknowledge the value of lived experience. That was the thinking behind the development of DIYAPS and low carb position statements. Acknowledging PWDs’ right to choice of treatment truly does put us in the centre of the discussion.
I should say that I am not undermining that leadership that organisations and individuals show when taking on these issues. It does take people to run with the ideas and turn them into something – whether that be a position or guidance statement, or different service or resource. I admit to occasionally feeling a level of frustration that legitimacy of some of these important-to-the community issues only comes when they have been made ‘official’ by an organisation, but I also know that all stakeholders involved is important; that together we are stronger!
Last week we saw on show discussions that have their foundations very much in the community. They may have moved into the realm of HCPs and researchers, and the conference stage. But it is well worth remembering where – and why – they originated.

DIYAPS – started in the community and now on the program at ATTD!
DISCLOSURES
I was an invited speaker at #ATTD2020, and my registration was covered by the conference organising committee. My airfare and part of my accommodation to attend ATTD was covered by Lilly Diabetes so that I could participate in the DOCLab advisory group meeting which took place on Friday, Saturday and Sunday. Other accommodation was covered by DedocLabs (I am an advisor for the #dedoc° voices program) and Novo Nordisk (I am a member of DEEP). I have not been asked to write or speak about any of the activities I attended, or anything I have seen at the conference.
The IDF Congress proved once again that the power of peer support should never, ever be underestimated. From spending time with the considerable number of diabetes advocates floating around the conference centre, to hearing about their work, to seeing them present their sessions, to speaking with the enthusiastic IDF Young Leaders, there were constant reminders of just how much we value and need contact with those who know diabetes.
Our peers are not only those whose beta cell production is on strike. It’s also the people who cheer and champion us. While I will always shout about how I need to be around others with diabetes – those who intrinsically ‘get it’ – my tribe also includes people affected by diabetes in other ways. Having friends and colleagues Taryn Black and Jane Speight at the Congress was wonderful because they were able to showcase the amazing work they do that champions people with diabetes. (They may not want to be friends anymore after they see this picture…)

When we asked for topic submissions for IDF2019, peer support rang out strongly as a topic for which there was much interest. This has been consistent with all the IDF Congresses I’ve attended. But we wanted to make sure we were considering it lots of different ways and at different stages of a person with diabetes’ life. What were the benefits for younger people with diabetes through their own eyes? We don’t get to hear from them all that frequently. And what about for older people who have lived with diabetes for many years, or who are newly diagnosed with diabetes? And what about people whose diabetes doesn’t neatly fit into the pigeonholes we so like to use in the diabetes landscape?
And so, the program managed to highlights these different aspects of peer support, showing that there are just as many ways we find a way to connect as there are people with diabetes!
So, here are some snapshots from different folks at the Congress to give you an understanding of just how much peer support was all around!
Lydia Parkhurst spoke about how important it was to have met other young people with diabetes as she moved from adolescent to young adulthood. She said: ‘It’s great having the support from my friends and family, but unless you have diabetes yourself, you never truly know.’

Georgie Peters looked at not only the positive aspects of peer support, but also how it may enable damaging behaviours – in this case, referencing recovery from a diabetes-related eating disorder.

Jane Speight spoke about how peer support may help reduce diabetes distress, and in my N=1 example, I can say that is certainly true.

Bastian Hauck acknowledged the input of peers in the #WeAreNotWaiting movement, explaining how the online support is the best 24 hour customer service hotline imaginable!
Cheryl Steele echoed Bastian’s comments about the DIYAPS online world in her talk that touched on support as she discussed the ages and stages of type 1 diabetes.

At the Ascensia Social Media Summit, in his opening remarks Joe from Ascensia made the point: ‘Peer support is a really important aspect of living with diabetes.’Ascensia’s commitment to this in their regular summits, as well as their online campaigns is brilliant. At this summit, there were 171 years of diabetes lived experience in the room, and a lot of camaraderie. There were a lot of buzz at this event, with people who had only known each other online suddenly becoming IRL friends.

Friend and fabulous diabetes advocate Phylissa Deroze spoke that not all peer support is right for all people. Finding space when living with type 2 diabetes can be challenging.
And peer support researcher and staunch supporter, Ed Fisher amended his well known ‘Four Key Functions of Peer Support’ by adding a fifth: ‘Being there and shared experience’. How wonderful is it that recognition of that ‘we get it’ aspect of peer support is being acknowledged by researchers?!

Off the program, it was impossible to ignore the power of that shared experience. We heard stories that resonated because they mirror our own. And then we heard those that were not anything like ours, but we wanted to learn more and understand just how they impacted our brothers and sisters with diabetes. When I heard Sana from Pakistan explaining the discrimination and stigma associated with diabetes means that women don’t tell their husbands they are living with diabetes, hiding away the day to day tasks required (if doing them at all), her advocacy efforts became even more remarkable. And when one of the young leaders echoed this story, and went on to share how she wore her pump prominently at an extended family gathering, despite warnings from her parents that it wasn’t a good idea, we couldn’t help but applaud. Feminism and diabetes activism is really tough going, and these were just two women being the change and storming the way through for others.
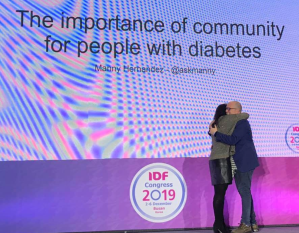
And, then…then there was Manny.

Manny Hernandez gave the award lecture for the Living with Diabetes Stream. When we were choosing who to acknowledge for this award, Manny stood out for his work in the diabetes community.
Manny was asked to choose his own topic for his talk, and came up with ‘The Importance of Community for People with Diabetes’. He couldn’t have chosen a better subject matter! Manny started by sharing his own story, and how it wasn’t until he met others with diabetes that he felt connected to a community. ‘I learned more in one hour with peers than in the previous four years,’ he commented. And then: ‘There are amazing endocrinologists out there but they can’t know what it’s like to live with diabetes, what the nuances of high and low blood sugar feels like, because they don’t live it.
Manny being Manny didn’t just leave it there. He wanted others to have what he had found, and so he created Tu Diabetes, followed by Es Tu Diabetes and The Diabetes Hands Foundation (DHF). For so many people with diabetes, this was a first foray into peer support. I know that it was a hugely valuable source of information and support for me. And it introduced me to people who have become very, very dear friends. (Massive shout out to Melissa Lee who was interim CEO of DHF after Manny left. I can’t even begin to explain how much I appreciate her warmth, wisdom and wit. And friendship.)
Manny’s award lecture was a love letter to and for all of us who have found that support which makes our lives with diabetes easier, better and more hopeful; for finding out tribes, loving them hard.
It’s no wonder that #PeerSupport was one of the most used hashtags at the Congress. It was recognised by speakers in different sessions as a cornerstone of diabetes management, just as important as other aspects involved in our care.
And so, I guess that this blog isn’t anytime soon going to stop or slow down extolling the benefits and value of peer support. Thanks to all those wonderful peers – friends – at #IDF2019 for making the experience such a rich and supportive one.
DISCLOSURE
I was the Chair of the Living with Diabetes Stream at the IDF Congress in Busan. My flights to Busan were covered by Ascensia Global (in order for me to get to Busan in time to co-facilitate their Social Media Summit). Flights home and accommodation were covered by the IDF.
Who wants to get out of a warm hotel bed and wander through the freezing streets of Busan to the BEXCO conference centre on the last day of an exhausting conference to be ready for an 8.30am session on diabetes and sexual health?
As it turns out, a lot of people do (including a few people who may have been doing karaoke until just a few hours earlier).
The symposium was in three parts. I started by talking about the female perspective of diabetes, sex and sexual health, followed by Grumps (Chris Aldred) giving the male perspective. Brilliant physician and academic, Fauzia Moyeen, closed out the session by highlighting current research in this area of diabetes.

Introducing Fauzia Moyeen to the stage.
My session at the IDF Congress focused on the recurring themes I hear from women living with diabetes. These themes were evident in responses to the blog post I wrote a couple of weeks ago asking women to share their experiences, and reinforced the messages I’d received after previous posts I’d published about diabetes, women and sex.
As much as I had wanted to present a variety of different experiences, the messages I heard from women was not especially diverse! Women from countries considered more liberal and open to discussions about sex said exactly the same things as out sisters from countries where you would expect limited information about sex and sexual health.
Over and over and over again, women echoed that they had never spoken about this issue with a healthcare professional, and if they had raised it, they were told diabetes does not impact on sex.
Some of the quotes were absolutely heartbreaking. Women shared stories of how their relationships ended because sex had become so painful and uncomfortable after their diabetes diagnosis and they had not been able to get help. One woman was told ‘…get used to it because that’s how it is’, another was told the pain was not real.
The emotional impact of feeling that yet another part of our bodies is letting us down and not doing what it is meant to is never considered or discussed. We are left to flail around with these intense feelings and concerns. It’s not even a matter of being able to get help – we don’t have anyone signal to us that this could be an issue.
Then there is the mess of adding hypos, or fear of hypos into sexual activity, or trying to be intimate when we’re hyper and our bodies feel leaden and achy. There is so little that is sexy about diabetes, and that may be especially true when we are trying to be our sexiest!
And then there is the whole contemplation of how to introduce a new partner to devices stuck on bodies and scars on skin, and the worry about how that will make them see us.
Discussion after my talk was lively, with HCPs asking some great questions. One wanted to know how to bring up the topic, which is really important. Many people are not comfortable talking about sex and sexual health. Not everyone is happy to share when they are experiencing problems. Cultural considerations come into play here as well. Having a HCP of a different gender speaking about sex makes some people very uncomfortable. One HCP said that when he has raised the topic, he’s been told that it’s none of his business.
I had some suggestions about normalising discussions about sex, while remain sensitive to people with diabetes, allowing them to dictate if this is a topic for discussion.
I believe it is essential that the person with diabetes is the one who decides whether or not sex and sexual health are to be topics of discussion. Now that doesn’t mean HCPs don’t get to ask at all, leaving all responsibility to the PWD. They can provide prompts. Perhaps have some brochures in the waiting room that can be accessed by women. (Yes! There are such things and you can see them here.)
Also, list sexual health and sex as something that may be affected by diabetes in general diabetes discussions. Think about it as a complication of diabetes and address it as you would any other complication. Just mentioning it plants a seed for the PWD to understand that this may be something that needs attention.
I borrowed a suggestion I heard Sarah Le Brocq during her language and obesity talk at the DEEP Summit earlier this year. Sarah shared how one GP practise has a little form for people to fill in before they go to see the doctor. There are a list of different issues and the person can tick the topics they are comfortable having discussed in the appointment. (This, she said, is a brilliant idea for people living with obesity, because often that is the first and only thing the doctor wants to speak about, even if the reason for the appointment is a sore finger or something irrelevant to the person’s weight).
Translated for diabetes, develop a checklist with potential topics, with sex as one of them. If the box had been ticked, that would signpost to the HCP that this was a topic that the person with diabetes wanted to discuss.
Another question came from a doctor who asked how to make discussions about sex a priority when he needs to focus on diabetes-related complications. ‘If a person is dead from a heart attack, sex won’t matter,’he said.
The response from people with diabetes was the same. Consultations need to focus on the issues that matter to people with diabetes, not tick the box exercises so HCPs feel that they are getting in all the things theywant to speak about.
Yesterday, I wrote this in my post:
‘… sometimes the chasm between what people living with diabetes want and need and what HCPs and researchers think we want is gulf-like.’
I felt that keenly after my talk. Women had told me that relationships had ended because of how diabetes had impacted on their sex lives. Others said that the discomfort they felt having sex meant that they just didn’t want to, and it had become a constant source of tension between them and their partner. Other women felt that they were failing themselves and their current or potential partners. One woman said that she refused to have sex because she didn’t want anyone to see how diabetes had marked her body.
To me, these sound like issues that need to be addressed, as much as, if not more so, than trying to adjust basal rates. They are just as important as making sure someone is doing their foot checks. They are far more important than knowing a current A1c. Dismissing the importance of sex in a woman with diabetes’ life as less critical than other aspects of her diabetes care clearly is doing us no favours.
The feedback following the session was really positive and I hope that we start to see similar sessions on programs at other diabetes events. Let’s get the dialogue happening so that women can feel comfortable talking about diabetes and sex. And get the help we may need.

DISCLOSURE
I was the Chair of the Living with Diabetes Stream at the IDF Congress in Busan. My flights to Busan were covered by Ascensia Global (in order for me to get to Busan in time to co-facilitate their Social Media Summit). Flights home and accommodation were covered by the IDF.

 It’s great that a number of PWD already know that they will be part of ATTD this year, attending satellite events run by different device and drug companies. Some are on the program and some will be there through other opportunities and work.
It’s great that a number of PWD already know that they will be part of ATTD this year, attending satellite events run by different device and drug companies. Some are on the program and some will be there through other opportunities and work.






