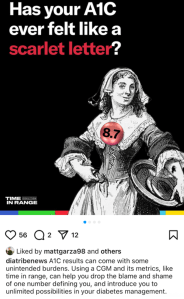
Earlier this week, diaTribe shared this on their Instagram:
It did not sit well with me at all. And I don’t understand the reference to stigma.
A1C is flawed. People with diabetes have been saying this for decades. To have our overall diabetes management measured by an average that gives no nuance to other factors is not a good way to assess health or guide treatment.
CGM changed all that, with visibility into just what is going on with glucose levels at all times. I finally understood why I was so tired some mornings, despite eight solid hours of sleep with in-range numbers at bedtime and at waking. I saw the rollercoaster nights, or the hours at time I was low. It became very clear that my nighttime glucose adventures were exhausting me.
As more people had access to CGM, TIR was heralded as the new gold measuring standard. And it was everywhere. I wrote and spoke about it a lot because the real-time data gave me a clearer understanding of my diabetes. But with that excitement came a gnawing discomfort: were we just swapping out one metric for another?
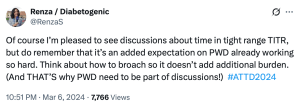
After a couple of years of TIR, and with the advent of newer, smarter AID systems there was a new kid on the block: Time in Tight Range (TITR). Target upper and lower limits were tightened and there were expectations of remaining within those ranges.
I nodded along because I was, for the most part, comfortably sitting within those number thanks to Loop. And yet, my discomfort grew. More pressure, more expectations on people with diabetes based solely on numbers, and a continued widening of the gap between people with access to tech and those without.
At ATTD a couple of months ago, there was the announcement of a new metric: Time in Normo-Glycaemia – TING! (There is no exclamation mark after the acronym, but it reminds me of the celebratory sound my kitchen timer makes when a cake is done baking, and that deserves festive punctuation.) And horrifyingly, to this #LanguageMatters boffin, the new acronym includes the word ‘normo’. Language position statements have always, always advised against using the word normal/normo. The word shapes attitudes that contribute to stigma. In one study, 85% of PWD surveyed found the word unacceptable.
These measures still focus on one thing: our glucose numbers. There are goals for the percentage of time each day we should be aiming to be in (ever-tightening) range. So, effectively, the HbA1c percentage has been replaced with time in range percentage. It’s still focusing on nothing more than numbers. It still sets us up for a pass/fail framework.
A1C, in itself, is not stigmatising. It’s a number. The language used when discussing A1C can be stigmatising. Attributing success in diabetes to an A1C number can be stigmatising. Being told we’re failing for not reaching an A1C of a certain number is stigmatising. But all of those things are true of TIR.
Before anyone comes at me and tells me that PWD should be able to have numbers within a tight range, of course that’s true. But isn’t that already the goal of our diabetes management? Isn’t that the point with all the glucose measuring, insulin dosing, and considering the bazillion other things we do to manage diabetes? I don’t know anyone with diabetes who does the work with a goal of glucose number of 17.0mmol/l; an HbA1c of 14%; a TIR/TITR/TING of 11%.
But replacing one measure for another still traps us in a numbers-only mindset. How is ‘What’s your TIR?’ really any different to ‘What’s your A1C?’ Does it free us from being metrics-focused? (Some might argue that it ties us to numbers even more with daily updates about how we’re tracking.) Does it address stigma?
I’m not sure it does. I’m not convinced that there is any relevance at all to stigma in this conversation. And I’m a little annoyed at the conflation. Diabetes-related stigma is very topical now, thanks to important efforts by PWD, community groups, researchers and clinicians in the diabetes space. If I was being cynical, I’d suggest that this is an opportunistic attempt to jump on the buzz movement of the moment without meaningfully engaging with what stigma really is or how any type of metric can contribute to it, depending on how it’s framed and used.
Postscript – but possibly the most important part…
And finally, but perhaps most importantly: the very idea that we are suggesting this is the gold standard when it is inaccessible to the vast majority of people with diabetes is just so out of touch. According to the diaTribe article that accompanied the Instagram post I shared earlier, worldwide 9 million people are currently using CGM as part of their diabetes management. The IDF’s latest Atlas data, (launched last month) reports that there are about 589 million adults (20-79 years) with diabetes across the world. That doesn’t include children and young people. (1.8 million young people are estimated to be living with T1D.)
Isn’t this one way stigma takes a hold? When we’re talking about targets that are only available to the small fraction of the diabetes community who can access the tools to achieve them. Setting standards around tech that most can’t obtain doesn’t just ignore reality—it reinforces the stigma of not measuring up.







1 comment
Comments feed for this article
May 28, 2025 at 10:22 am
Trish Riley
Yes I agree Renza. My clients are mostly older PWD who are fed up finger-stick testing and mostly do not understand that A1c is not BGL. I agree with the literature that older PWD who have embraced a trial with CGM love it and cope with it well, however T2D for many cannot afford it later and then feel cheated to not be able to access this tech (+ other tech) in a blessed country like Australia. TIR, TITR etc is wonderful and a far better metric, but for whom? They do the best they can, and if they are engaged with their cycle of care, that has to be good enough till anything changes.
LikeLike